Are You Or A Loved One Suffering From Depression, PTSD, Anxiety, or Bipolar Depression? Consider A Rapid, Effective Treatment That Works in 70% of Patients Within Days
What Is NOVA Health Recovery?
NOVA Health Recovery is focused on the treatment of mental health and addiction by using innovative, integrative therapies to manage conditions that are, at best, difficult to treat. For mental health disorders, we utilize traditional medications as well as ketamine infusion therapies for the treatment of:
Bipolar Disorder
Obsessive Compulsive Disorder
Anxiety
PTSD
Addiction
We also utilize ketamine therapies as infusions, topical lotions, oral lozenges, and nasal spray for:
-
Chronic Pain
-
CRPS
-
Trigeminal Neuralgia
-
Cluster Headaches
-
Phantom limb pain
-
Migraine Headaches
-
Post Herpetic Neuralgia
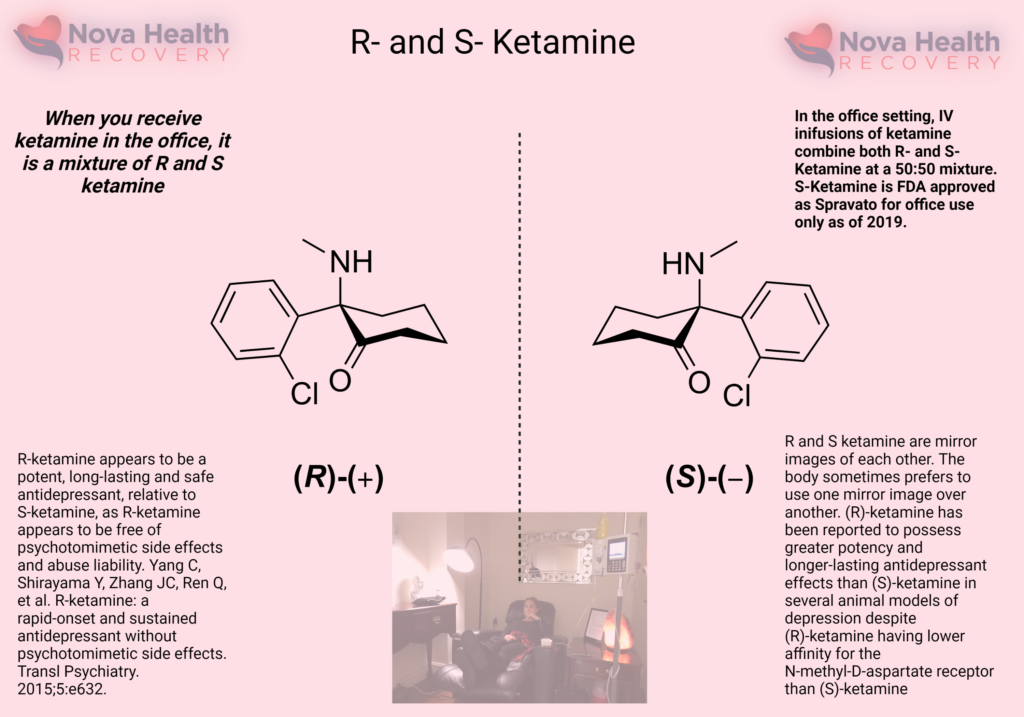
Ketamine, a fabricated chemical from the 1960’s, was FDA approved for anesthesia in 1970 and is listed as one of the safest drugs on the planet per the World Health Organization. The question of whether to use ketamine to treat your depression should not be a question of who should get the treatment but rather ‘why isn’t everyone getting ketamine treatment?’ As psylocibins are branded as ‘magic mushrooms’ and evoke mystical qualities, ketamine has unfairly been branded as a party drug or ‘horse tranquilizer.’ Yet, ketamine has been effectively proven to treat depression, mood disorders, and pain in numerous studies and is available to the public right now. Even with concerns over abuse and addiction, ketamine does not cause any traditional withdrawal symptoms which one would get from stopping cannabis or coffee. In fact, there is plenty of evidence that demonstrates the efficacy of ketamine in the treatment of addictions such as alcohol and opiate abuse.
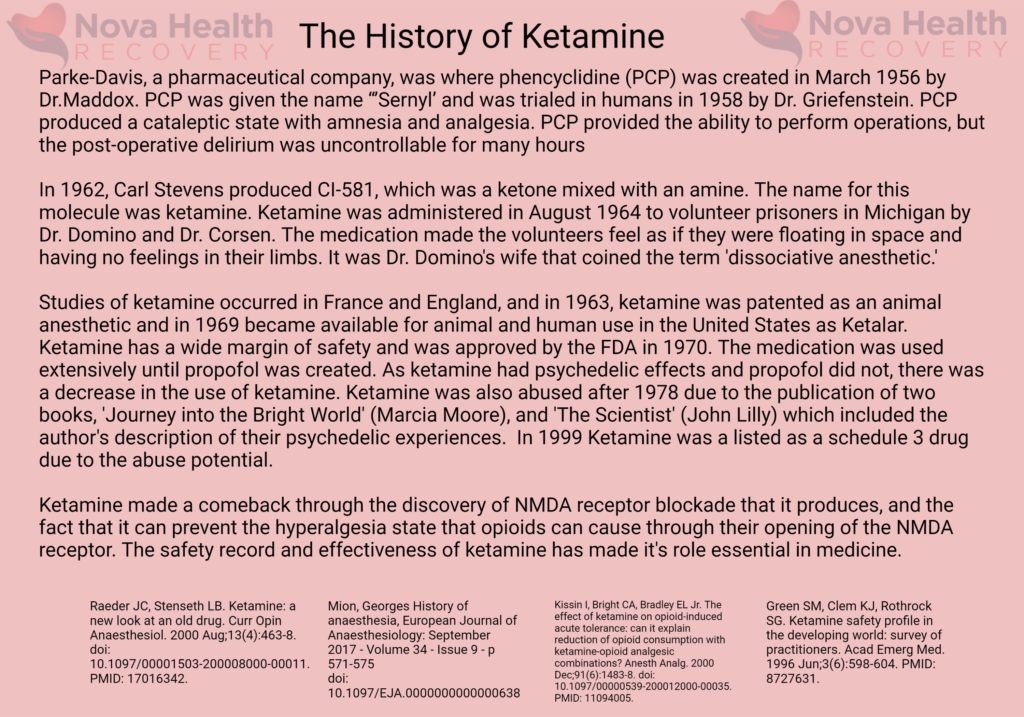
In 1956, a chemist (Victor Maddox) at pharmaceutical company Parke Davis in Detroit, Michigan was experimenting with synthesizing new compounds in an attempt to find a better anesthetic. A compound called phencyclidine was initially created, and in early animal studies it demonstrated unusual effects. Some animals exhibited a drunk-like state when administered with it, while others entered states of delirium.
Human tests quickly ruled out the compound as clinically useful with some patients exhibiting major delirious and dissociative states for prolonged periods of time. This was despite the fact the it did seem to function remarkably well as an anesthetic. In later years, phencyclidine hit the streets as a recreational drug, becoming infamous due it its violent side effects. Its street name was PCP, or angel dust.
In the early 1960s, Parke Davis researchers began searching for a phencyclidine derivative that could limit the compounds unmanageable side effects. It was here that ketamine was born through the work of Calvin Stevens and after successful animal tests, it was administered to the first human subject in 1964, demonstrating remarkable anesthetic effects.
Initially approved for veterinary uses, ketamine quickly found a place as an effective short-acting anesthetic and was approved by the FDA in 1970. One of its first major human uses was as a battlefield anesthetic in Vietnam. It has been suggested that this initial use in the early 1970s was what led to it moving into recreational circles as veterans returned to the United States and continued using the drug.
Non-medical uses continued throughout the 1970s, culminating in several high profile publications “outing” the drug. Perhaps the most infamous of these accounts came with scientist and psychonaut John C. Lilly’s 1978 autobiography The Scientist: A Novel Autobiography.
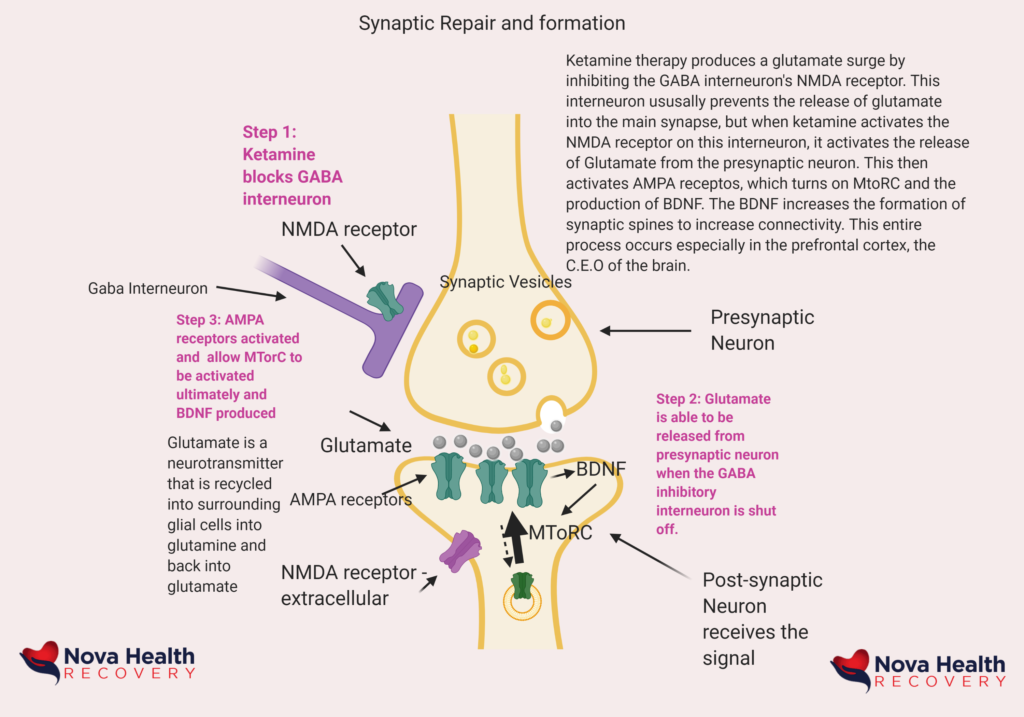
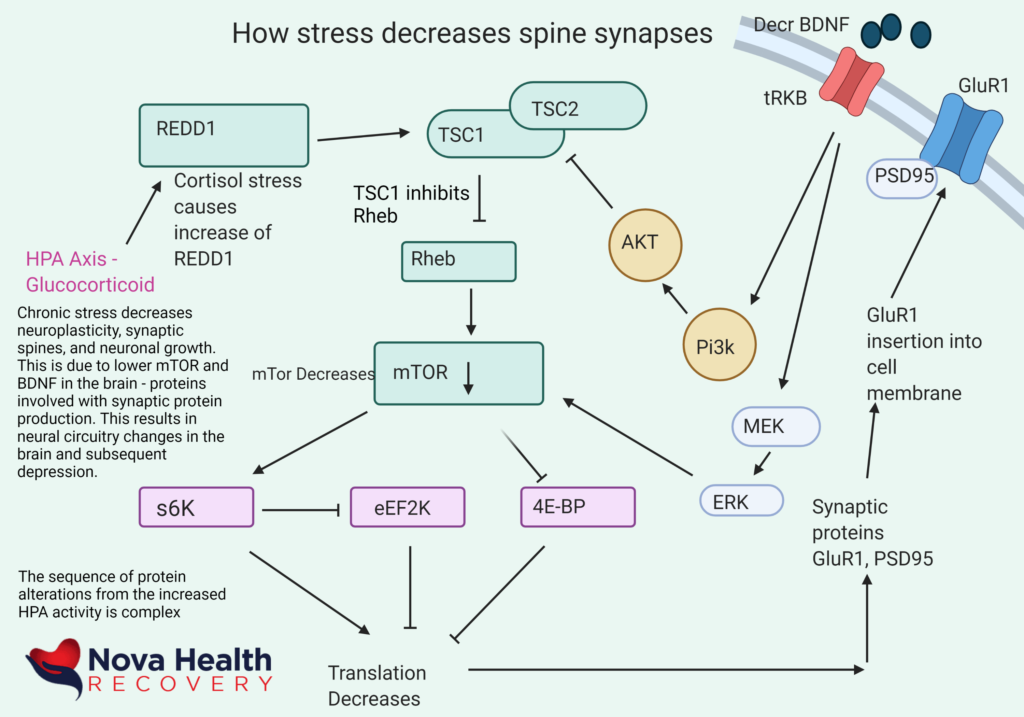
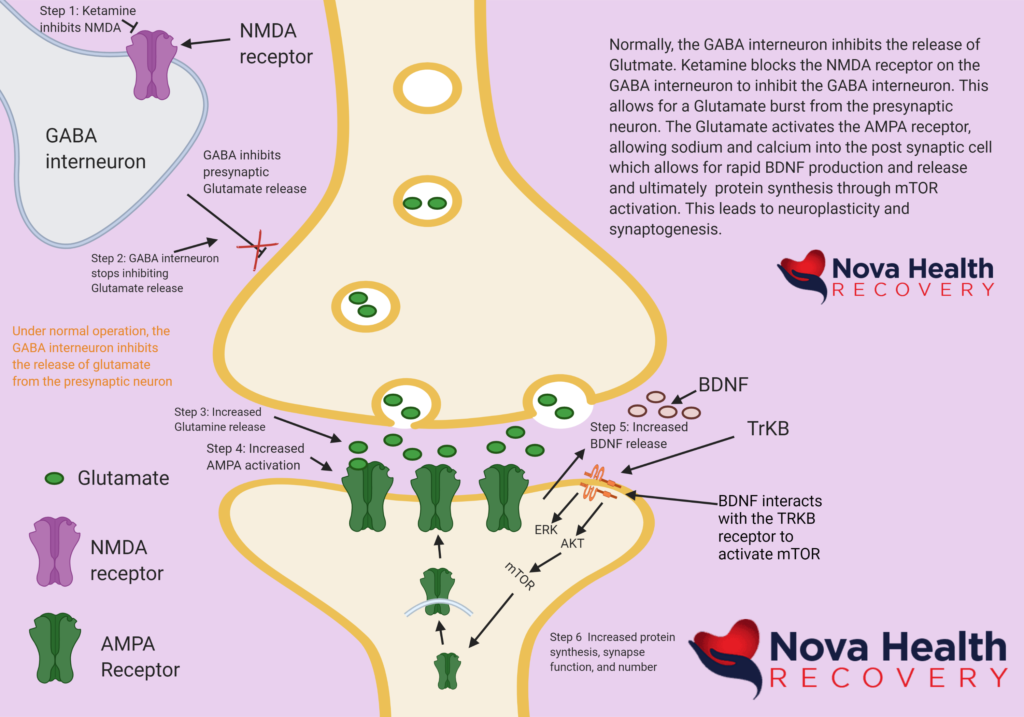
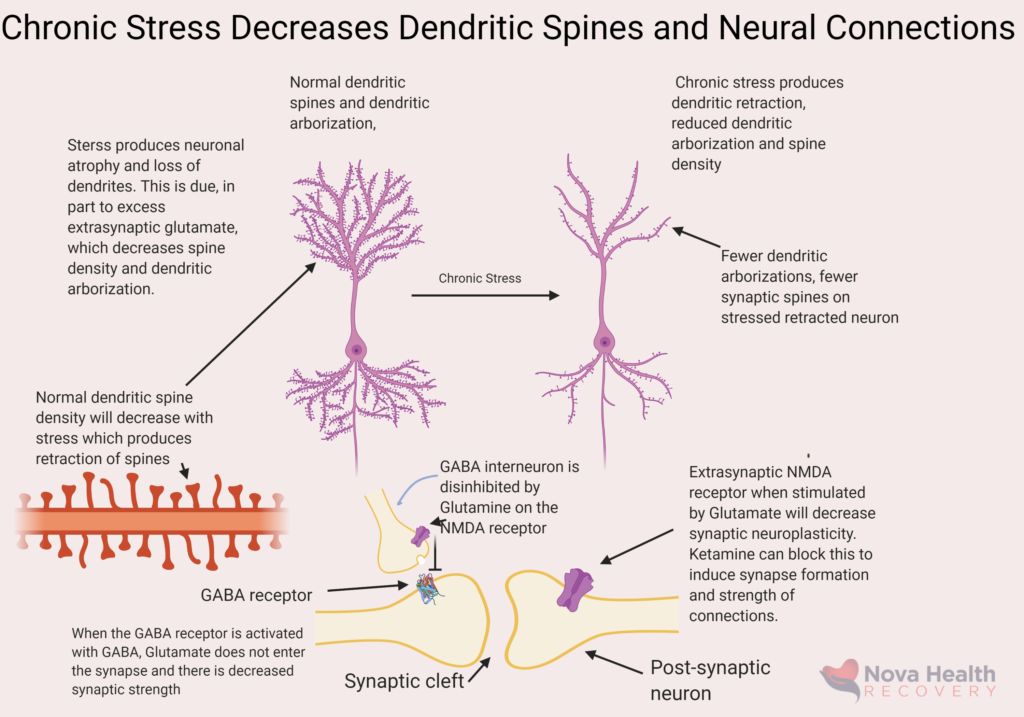
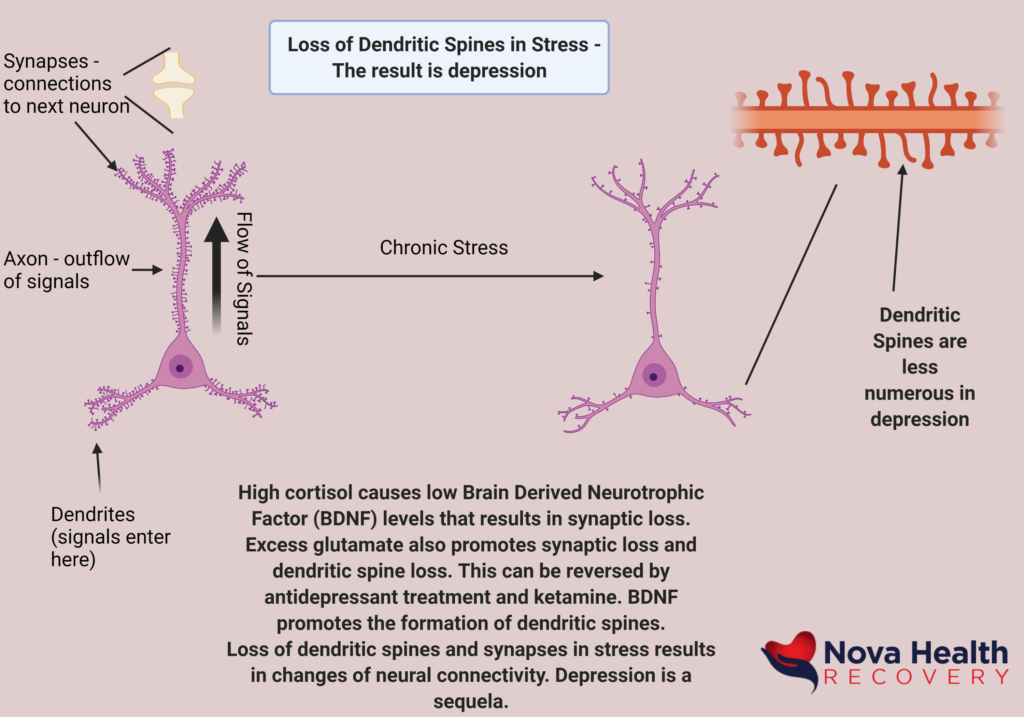
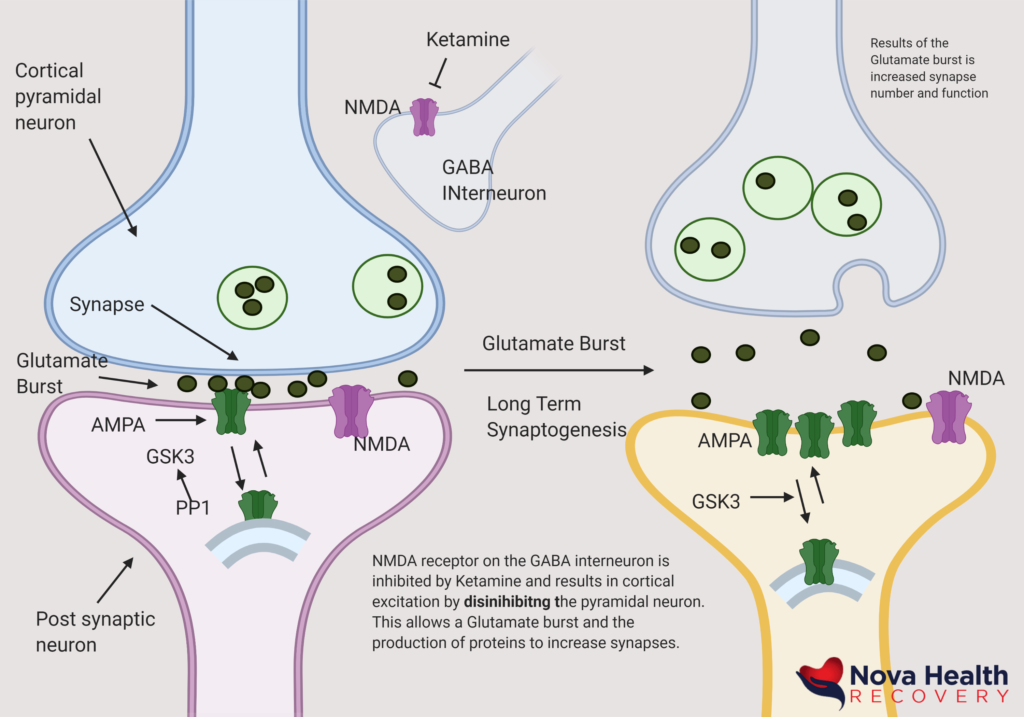
Ketamine works in numerous complex ways. It affects the glutamate system, which is the primary system of our brain involved with learning. Our entire cerebral cortex runs off glutamate as an excitatory neurotransmitter. It is balanced by GABA, which ‘calms’ the brain down. Serotonin, the molecule of happiness, and dopamine, the molecule of reward, are more primitive transmitters and, in fact, serotonin is present in locusts and causes them to swarm. These more ancient neurotransmitters are, in part, controlled by the functioning of the glutamate system, especially through the amygdala (the anxiety center) with the lateral habenula, both of which stop the release of serotonin and dopamine when there is excess glutamate. The glutamate system is the primary neurotransmitter in the cerebral cortex of mammals, and it effectively runs the ‘ecosystem’ of our brain, controlling most other operations. Excess glutamate can result in neuronal damage and death, loss of circuitry in the brain, and depression. Ketamine allows a brief glutamate burst and then shuts off the signal. This results in the formation of proteins and Brain Derived Neurotrophic Factor (BDNF) which in turn causes the production of dendrites and synapses (synaptogenesis) in neurons in key areas. This allows for the formation of new connections and new learning, which is a vital to its antidepressant effects. This is called neuroplasticity.
In effect, ketamine helps repair over-pruned neural circuits in the brain through the production of BDNF, new synapses, increased and strengthened neural connections, decreasing glutamate levels, shutting off the lateral habenula and amygdala to decrease anxiety, increasing serotonin and dopamine, and improving reward deficiency such that individuals feel more motivated and energetic. In fact, ketamine treats anhedonia, a situation in which the treatment of depression with typical medications results in no mood at all – no happiness or sense of fulfillment or excitement.
Glutamate and Neuroplasticity
Most of the cerebral cortex is run by Glutamate, a molecule of learning, and this is balanced by the neurotransmitter GABA. Glutamate bursts in the brain are excitatory and result in the production of new synapses or connections between neurons. The other name for this is neuroplasticity, and it is a key part of learning. We are always pruning our neural networks, creating new connections (dendrites and synapses) and increasing the number of neurons. This is part of the learning process, and this goes away in severe depression. This is why we frequently become vegetative when severely depressed, lying in bed all day, with our brain not really thinking of anything (paucity of thought). This is because the brain has shut down new learning due to lack of neuroplasticity. We move less, we think less, we sleep less (or more) and we feel anxious. We begin to ruminate over the same problems, which is the anxious side of our brain.
The Problem with Traditional Therapy
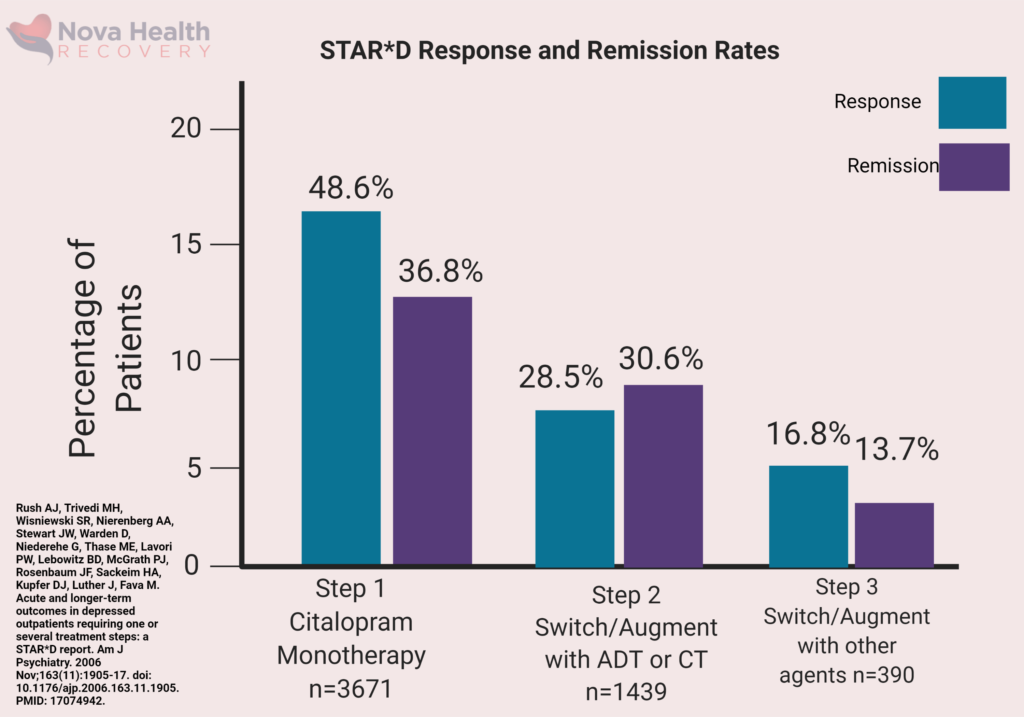
Traditional treatment for depression would include medications that frequently do not work in 1/3 of cases and may take months to begin to help. In addition, there are numerous side-effects of antidepressant medications, such as weight gain, impotence, and anhedonia. Anhedonia is effectively the state of having no mood, where there is no anticipatory reward nor is the person depressed. So, for some, they may become ‘undepressed’ after treatment, but they still cannot have a normal life because of anhedonia. They cannot return to work because of lack of motivation, energy, drive, and continued cognitive deficits as ‘brain fog.’ This is where some may lean on substances to help themselves feel better. The other issue with traditional medications is that they may take months to work. In the age of interventional psychiatry, this is too slow. Depression leads to poor functioning, brain fog, and irritability which impacts jobs, family, and personal goals.
Given the economic and personal damage that depression causes, why would anyone want to wait months to feel better? Ketamine offers a rapid response in days in over 70% of patients. In fact, mental health should be treated like an emergency, just like an infection or heart attack, with aggressive and rapid acting therapies because untreated mental health disorders increase medical risks, produce early death, and increase the risk of addictions. As a result, there is a decrease in quality of life, productivity, and personal fulfillment.
Depression Causes Cognitive Decline and Neurodegeneration - Brain Fog and Lower IQ
The Effect of Depression on your Cognition
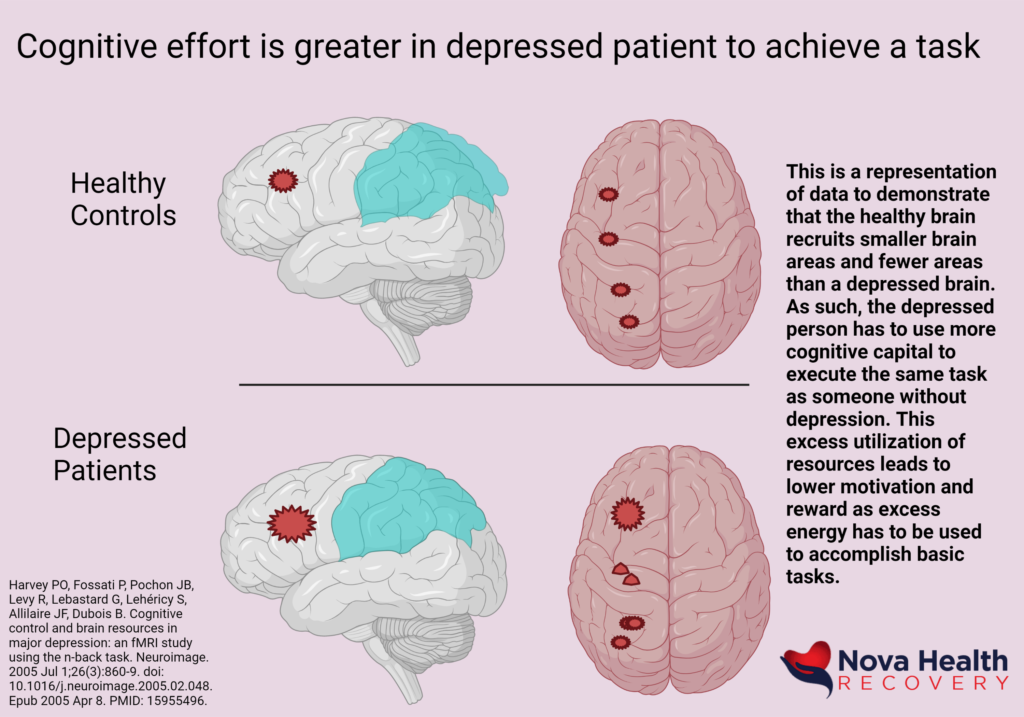
What many do not recognize is the impact that poorly treated depression has on cognition. There is a decrease in the functioning of neural circuits in the brain such that areas (the Prefrontal Cortex) involved in decision-making, executive functioning, and impulse control become damaged and literally shrink. Also affected is the hippocampus, which is involved with working memory. This results in brain fog, poor insight, and poor decision-making and is visible on MRIs of the brain demonstrating decreased brain volumes in patients with mood disorders such as depression. Areas of the brain that sense reward also are altered, and this affects happiness and motivation. The basic things in life, such as a good movie, a delightful book, or an evening out on the town are not enjoyable or rewarding. There is a reward deficiency. Think about even smaller rewards such as brushing your teeth, combing your hair, getting out of bed, or taking a shower. Anyone who has been depressed may have found it impossible to get out of bed, brush their teeth, or even take a shower. That is because there must be a reward value associated with these activities. For example, by brushing your teeth, you will keep your teeth healthy so you can eat a steak in 10 years. This requires the ability of insight and delayed discounting, which is the ability to see value in things that may become rewarding later, even if it is a small reward. For example, there is nothing rewarding about taking ocular vitamins as you do not see better the next day after you take them. This is where the prefrontal cortex tells us that we should take vitamins to save our eyesight or even exercise when the activity is less than pleasurable. When we get depressed, our ability to see the value in any task becomes exceedingly difficult. We lose the ability for delayed discounting and the motivation to do even basic things in life.
The anti-reward areas of the brain, in particular, the amygdala and lateral habenula, control our responses to anti-rewards, or things that can cause us harm. These systems of the brain turn off the deeper neurotransmitter systems such as dopamine, or reward pathways, and serotonin, or happiness neurotransmitters. In depression and anxiety, this side of the brain is frequently running non-stop and leads to the anxiety one frequently experiences in depression.
Depression and Stress Result in Loss of Brain Connections (Synapses)
Mood Disorders Are Neurodegenerative - They Shrink Key Areas of The Brain Due to Neuron Loss
Loss Of Brain Volume and Loss Of Neuronal Connection Results in Loss of Cognition - Brain Fog
Brain Fog Results From Loss of Neural Circuit Connections, Neurons, and Synapses
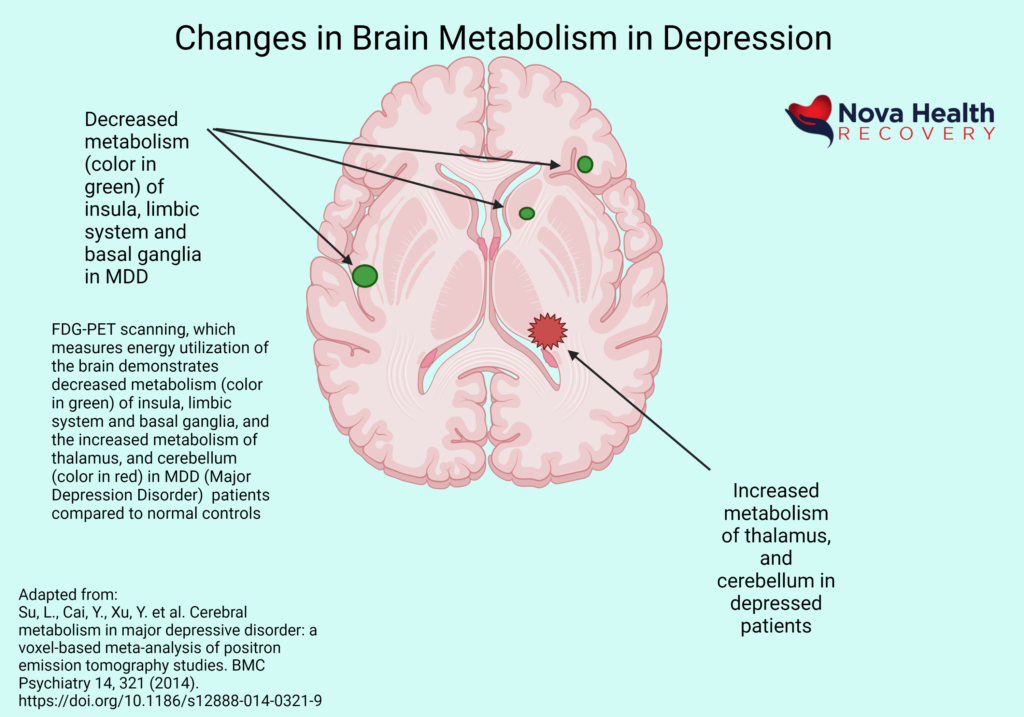
Brain Metabolism Decreases With Depression - This Causes Cognitive Decline and Low Motivation
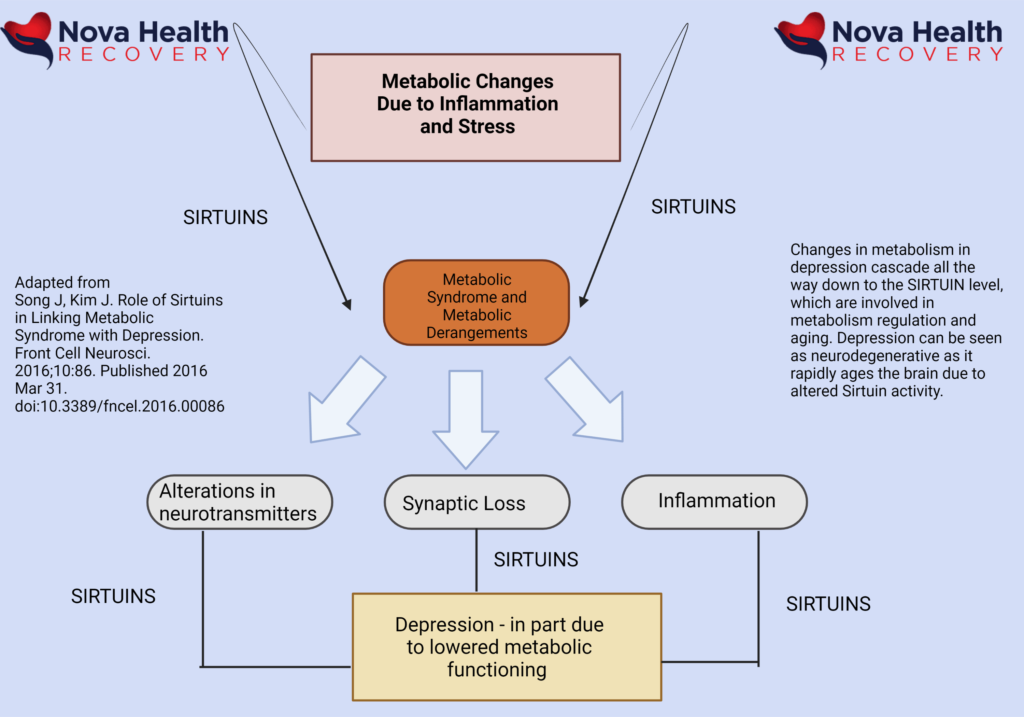
The Brain of A Depressed Patient Ages More Rapidly Due to Changes in Sirtuins
Glutamate is the primary Neurotransmitter in the Human Cortex - The Molecule of Learning
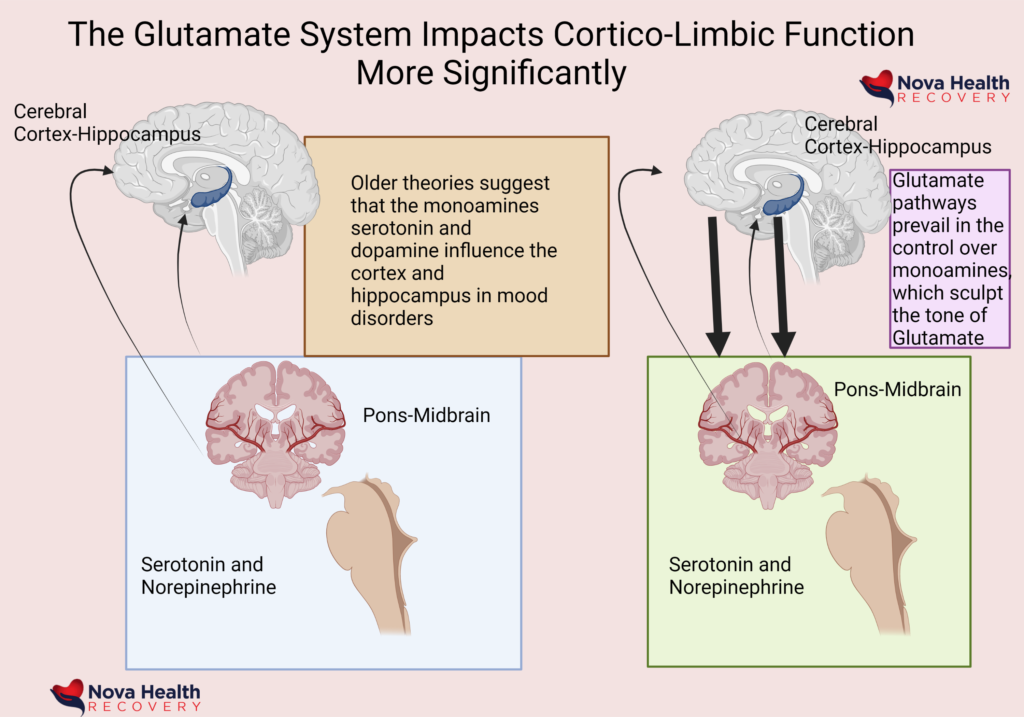
Glutamate and Neuroplasticity
Most of the cerebral cortex is run by Glutamate, a molecule of learning, and this is balanced by the neurotransmitter GABA. Glutamate bursts in the brain are excitatory and result in the production of new synapses or connections between neurons. The other name for this is neuroplasticity, and it is a key part of learning. We are always pruning our neural networks, creating new connections (dendrites and synapses) and increasing the number of neurons. This is part of the learning process, and this goes away in severe depression. This is why we frequently become vegetative when severely depressed, lying in bed all day, with our brain not really thinking of anything (paucity of thought). This is because the brain has shut down new learning due to lack of neuroplasticity. We move less, we think less, we sleep less (or more) and we feel anxious. We begin to ruminate over the same problems, which is the anxious side of our brain.
.
Increasing Brain Derived Neurotrophic Factor Is Key to Brain Health and Antidepressant Effects of Ketamine
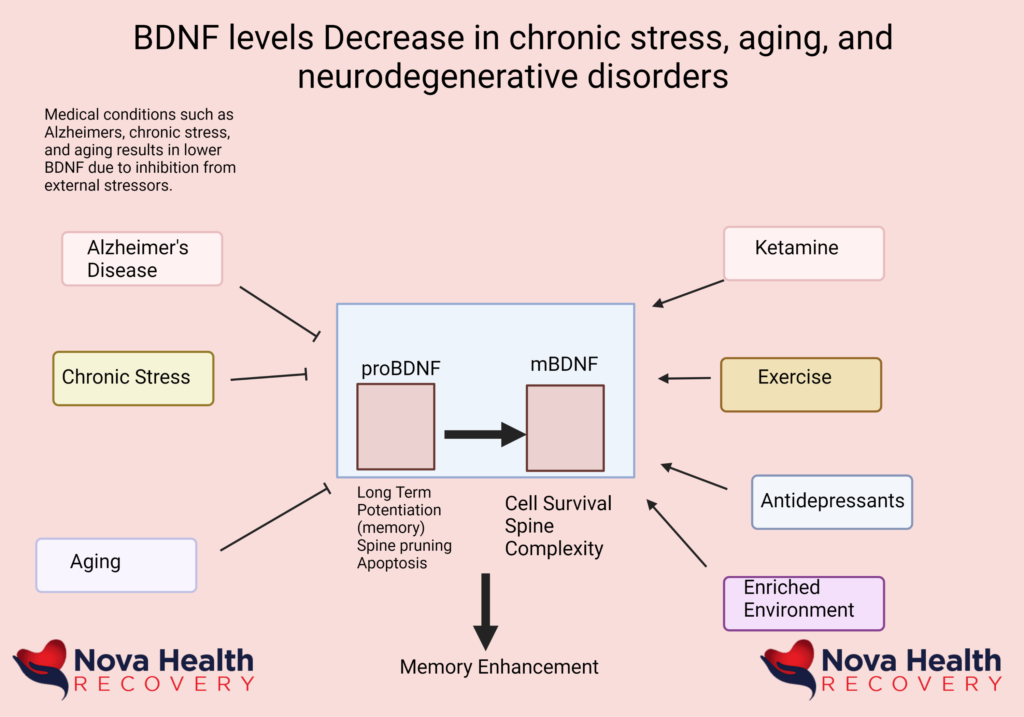
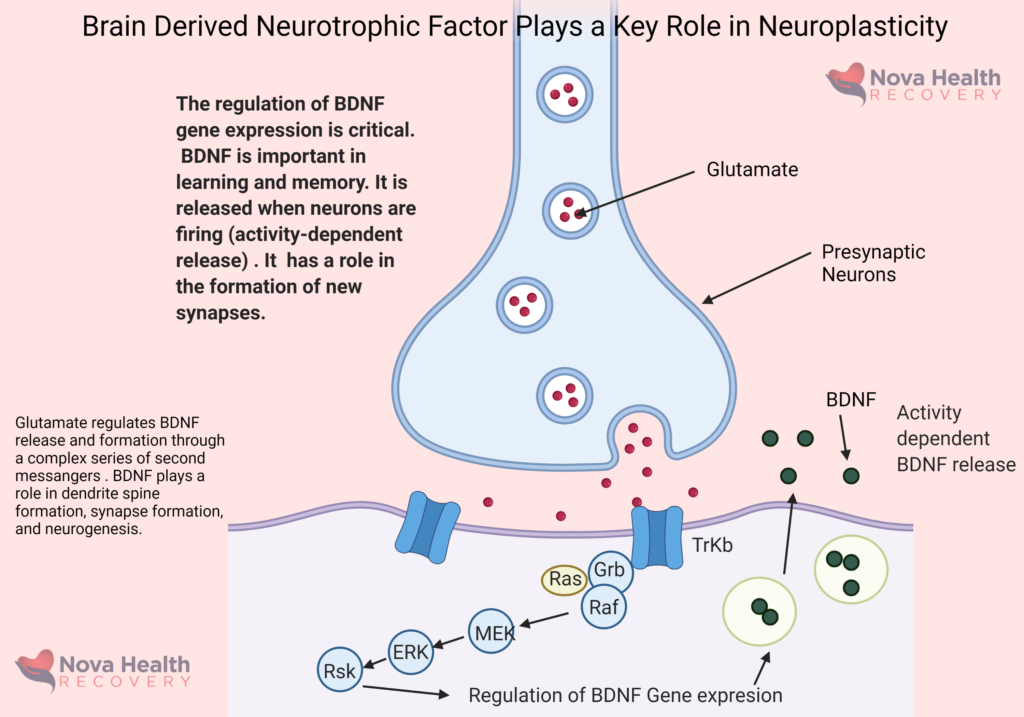
Ketamine Therapy Allows For Rapid Glutamate Signaling To Produce BDNF for Neuroplasticity
Traditional Antidepressants Fail to Work in 2/3 of Patients and May Take Months to Show Any Effect
The Problem with Traditional Therapy
Traditional treatment for depression would include medications that frequently do not work in 1/3 of cases and may take months to begin to help. In addition, there are numerous side-effects of antidepressant medications, such as weight gain, impotence, and anhedonia. Anhedonia is effectively the state of having no mood, where there is no anticipatory reward nor is the person depressed. So, for some, they may become ‘undepressed’ after treatment, but they still cannot have a normal life because of anhedonia. They cannot return to work because of lack of motivation, energy, drive, and continued cognitive deficits as ‘brain fog.’ This is where some may lean on substances to help themselves feel better. The other issue with traditional medications is that they may take months to work. In the age of interventional psychiatry, this is too slow. Depression leads to poor functioning, brain fog, and irritability which impacts jobs, family, and personal goals.
Given the economic and personal damage that depression causes, why would anyone want to wait months to feel better? Ketamine offers a rapid response in days in over 70% of patients. In fact, mental health should be treated like an emergency, just like an infection or heart attack, with aggressive and rapid acting therapies because untreated mental health disorders increase medical risks, produce early death, and increase the risk of addictions. As a result, there is a decrease in quality of life, productivity, and personal fulfillment.
The STAR*D Trial Demonstrated The Poor Performance of Traditional Antidepressants.
Depression and Mood Disorders Increase The Risk Of Heart Attack, Strokes, and Hypertension
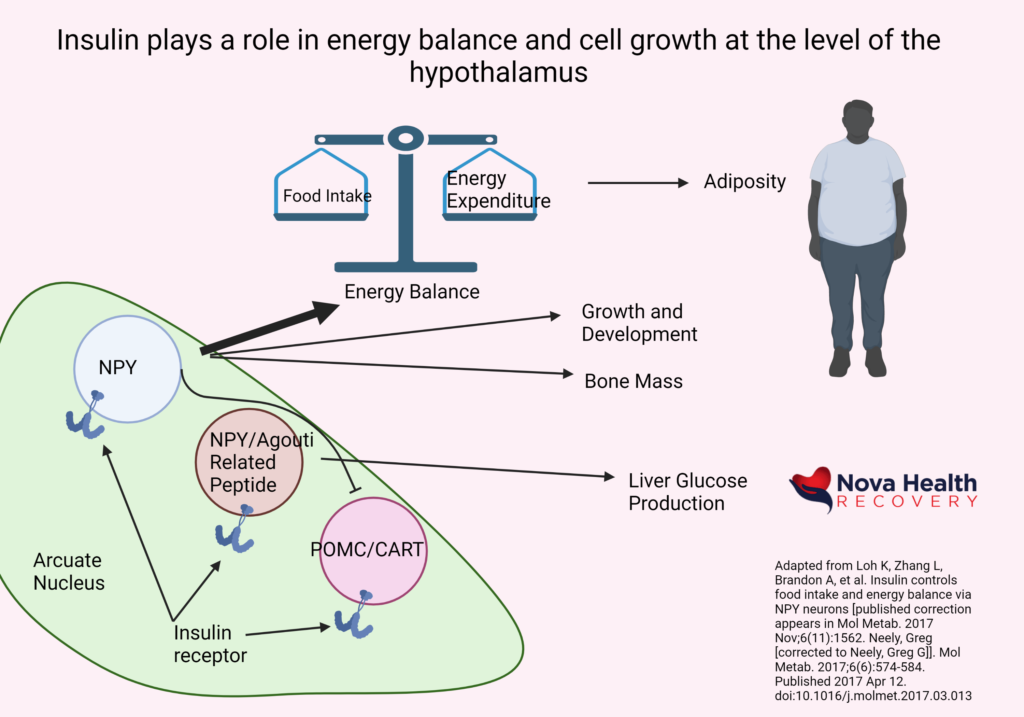
Changes in Insulin and Weight Are Associated With Depression and Low Motivation
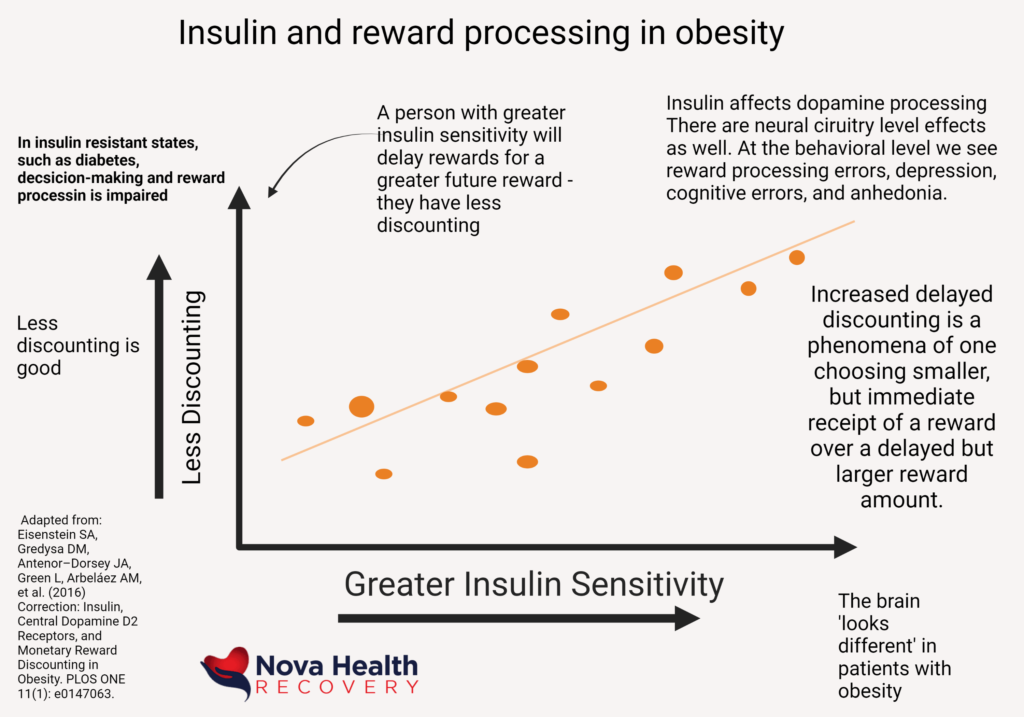
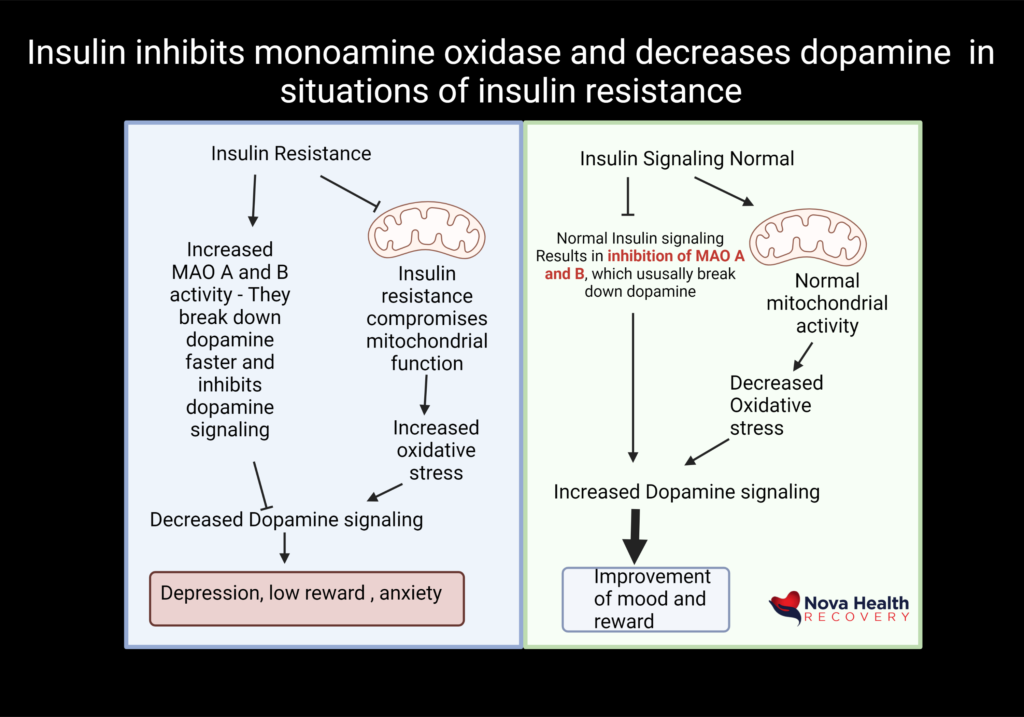
Obesity and Other Metabolic Factors Impact Brain Health and Depression - NOVA Health Recovery Ketamine Center Can Evaluate These As Well
Ketamine Therapy Should Be Considered Early For Depression Treatment And Prevent Further Neurological Decline
Why Ketamine Therapy Should Be Your First Choice
Ketamine offers rapid treatment with a prominent level of success of 70% in treatment resistant patients. Given the metabolic complications that mental health disorders produce as well as loss of work, family disruptions, and personal struggles, it would be appropriate to consider ketamine therapy as a first-line treatment. It is better to prevent damage than react to it. Ketamine can be used alongside traditional medicines or as a stand-alone therapy. NOVA Health Recovery Ketamine Center in Alexandria, Virginia offers evaluation of your mental health disorder, consideration for treatment options, including Ketamine, Nitrous Oxide, scopolamine, Low level laser light therapy, NAD+ infusions, and compounded therapies. We do use home-based oral ketamine and home-based ketamine nasal spray therapies for maintenance of depression treatment. Remember, ketamine is a treatment, not a cure, so just like your hair, you must comb it and wash it frequently – the same goes with mental health. You need to maintain the lifestyle of better mental health just like a weight loss program.
Ketamine is Part of a Lifestyle Change
Ketamine should be one of the layers of treatment in every mental health condition. We can refer you for continued therapy with psychologists who are familiar with trauma, addiction, and severe mood disorders. Cognitive Behavioral Therapy has a significant role. We can adjust your medications as needed and help treat side-effects from them. Proper nutrition, medical weight loss, intermittent fasting, supplements, guided exercise, high intensity interval training, saunas, Yoga, Tai Chi, Craniosacral therapies, and many other therapies need to be incorporated into your recovery. Structured time and Boredom need to be addressed as they are root causes of depression and addiction. For some, a life coach would be valuable. Evaluations for secondary causes of depression, addiction, and mental health can also be addressed and these include small bowel overgrowth assessments, organic acid testing, Lyme disease and babesiosis testing, allergy testing, mycotoxins, and organic pollutant testing, as well as genetic testing for drug metabolism and supplement choice. Laboratory testing for vitamin D, thyroid, vitamin levels, autoimmune panels, heavy metals, copper, acute intermittent porphyria, pyrroles, sex hormones, and other labs can be assessed as well.
Ketamine represents a huge step forward in the treatment of mental health disorders such as depression. Patients do not need a referral or psychiatrist, but patients with heart disease, kidney failure, liver failure, stroke, heart attacks, or schizophrenia would need a medical clearance for the procedure and treatment. The question of whether to get ketamine or not is simple: why wouldn’t a person want to get rapid results with a safe and available therapy when they have suffered so much? How has your mental health journey been so far? In minds that have fixed beliefs and cognitive rigidity where they cannot think creatively, the mantra of ‘that didn’t work the first time…let me try that again….and again….” tends to be an ongoing process. Not making a decision is actually making a decision to not consider therapies that may change your life. Everyone needs a push. Hopefully that choice is made early. You have to challenge yourself to change yourself.
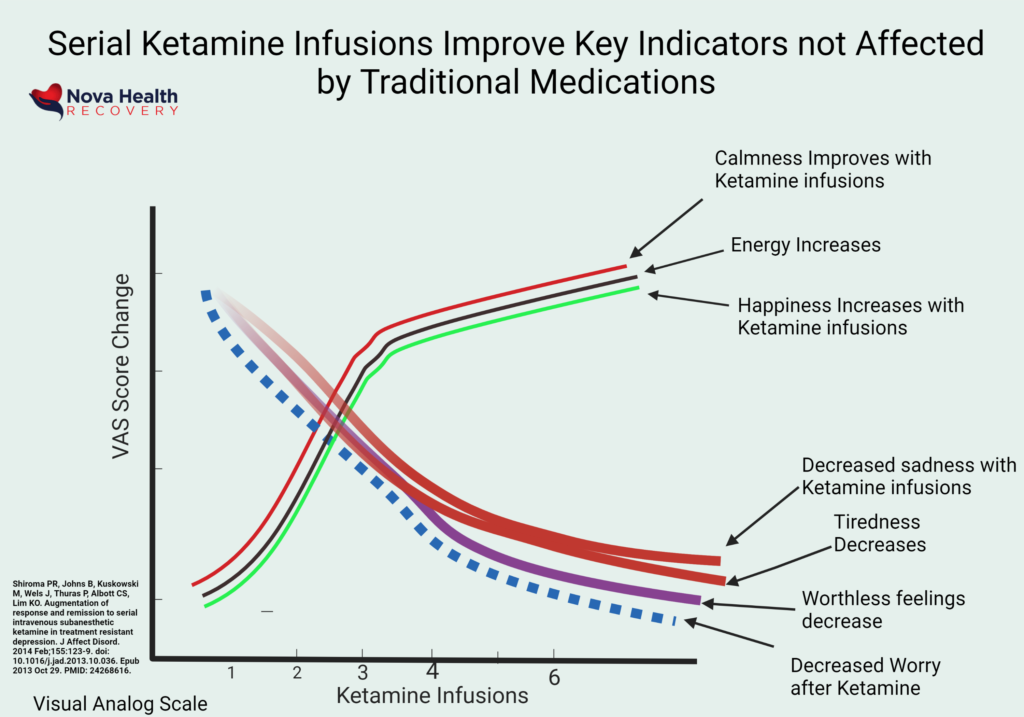
Ketamine Therapy Improves Wellness Parameters That Traditional Medications Do Not: Such as Happiness, Hope, Motivation, Reward, Fatigue, and Energy.
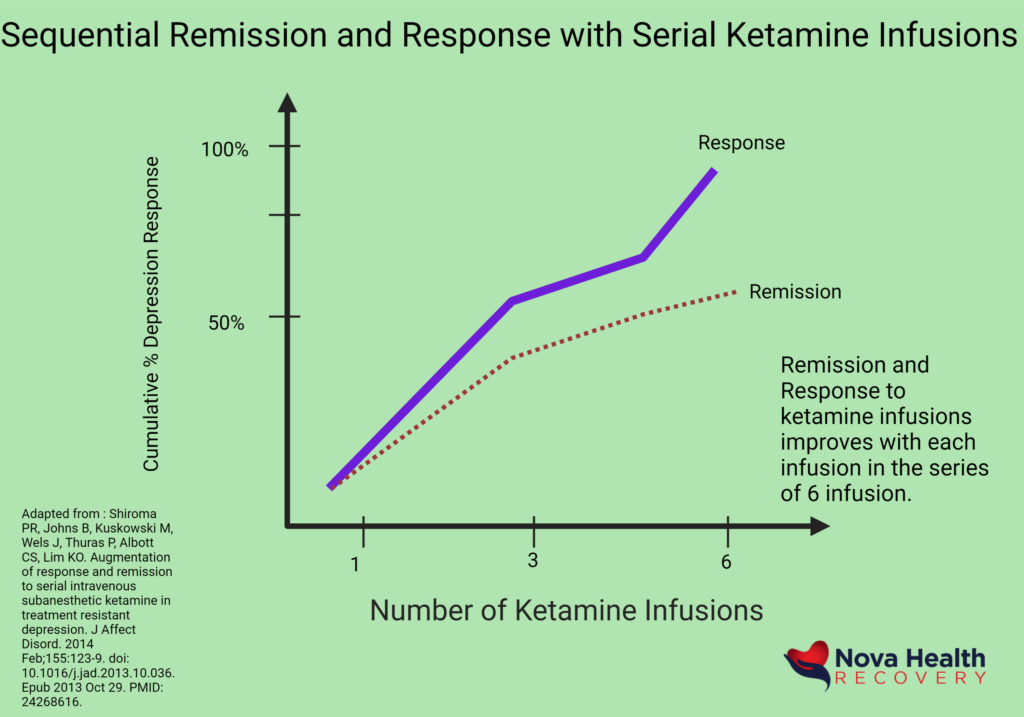
Sequential Ketamine Infusions Results in Remission or Response in over 70% of Treatment Resistant Patients
What are the steps for Ketamine Therapy Treatment?
The condition that is being treated must be appropriate for ketamine. We evaluate this with our initial phone consultation with the individual. The level of expectations for results and need for ongoing maintenance therapies are discussed.
Conditions Does Ketamine Treat?
-
Multiple Painful conditions
-
Suicidal Thoughts
-
Pain
-
CRPS | RSD
-
Fibromyalgia
-
Cluster Headaches
-
Chronic Fatigue Syndrome
-
Neuropathic pain
-
For Mindfulness, hypnosis, guided imagery
-
Post-herpetic neuralgia
-
Phantom limb pain
-
Initial Depression Treatment – Augmenting Traditional Medications to make them work faster
Ketamine is a treatment that will make underlying medications work better, allow an individual to succeed in their traditional psychotherapies, or allow one to diminish medications that may be causing side-effects. For some conditions, such as depression, statistically significant benefits can be mentioned, such as 70% of patients have improvement of remission in their depression. On the other hand, for other conditions, such as OCD and chronic pain, the established data is not so clear.
Who can receive ketamine therapies?
Anyone is a candidate if they are medically stable. If there are medical issues, a medical clearance may be needed.
Who Will Need Medical Clearance Prior to Therapy?
-
Cardiac History
-
Stroke History
-
Liver Failure
-
Dialysis or Kidney Failure
-
Schizophrenia
-
Allergy to Ketamine
-
Uncontrolled Hypertension
Do I need a Referral?
NOVA Health Recovery Ketamine Center does not require a referral, but some medical problems may require further evaluation before the treatment is started. We can manage medication adjustments and set up follow-up therapist visits. We can also address and treat mental health conditions such as ADHD, depression, and anxiety with traditional medications.
The Consultation Process
In order to assess whether Ketamine is the right choice for you, we conduct an initial mental health screening using various questionnaires and a comprehensive assessment. We assess cognitive loss with screening tests as well as lifestyle modifications and supplements that can enhance the outcome of therapy. We can address substance use disorders, pain, and obesity-related issues that can be involved with mood disorders. The consultation involves a deep dive into your mental health journey as well as evaluating medical conditions and lifestyle choices that can impede recovery.
The Preparation Process
It is best not to eat for four hours prior to the visit. Liquids are fine. Take your usual medications. Medications such as Clonazepam, Ativan, and Lamictal are fine to take as well and should not be tapered as that will cause more distress. Keep your usual doses of medications the same.
Clear your mind of any stress. Unload your schedule or routine of excess tasks for the day,
Prepare an ambient musical selection or a ketamine playlist
Find eyeshades, weighted blanket, and noise cancelling headsets.
Focus on one issue that you may want to resolve.
Remember that neuroplasticity is what you want, and that occurs whether you have an excellent infusion experience or not. You do not have to dissociate to have efficacy.
Therapy sessions are best done the day after an infusion.
The mood elevation and dissociation of the infusion is a side-effect of ketamine and not the cure. Neuroplasticity is the result.
.
The Infusion Process
After the initial assessment, we will schedule your infusion sessions, which generally can start the same day if appropriate. Before receiving each infusion, we will need to verify that you have arranged transportation (such as family or an Uber) in order to leave the clinic as you will not be able to drive for the next several hours until the effects of Ketamine wear off.
On the day of the infusion, patients will be taken into an exclusive infusion area. An I.V. will be started as painlessly as possible, using cold spray if needed. We utilize exceedingly small I.V. needles typically used in pediatrics. We will check your vital signs and answer any further questions. During the procedure you will be lying in a comfortable lounge chair for the entire duration of the 45-minute infusion sessions. We can offer Ketamine Assisted Psychotherapy for an additional fee, or you can even have your own therapist join you for your session. We utilize Phillips Hue lighting, aromatherapy, as well as ambient music through a SONOS system for those who do not headsets. It is good to use noise cancelling headsets to prevent any extraneous sounds from affecting your experience.
How Often do I Need to Receive an Infusion of Ketamine?
Initially the series of 6 is used for depression, anxiety, OCD, and bipolar disorder. These are done twice or three times a week. It is best to not let more than 5 days go between infusions. CRPS and neuropathic conditions may require multi-day 4-hour high-dose infusions.
What Does a Ketamine Infusion Feel Like?
Each infusion is different. We initiate doses at a therapeutic level of .5 mg/kg IV of ideal body weight over 40 minutes. Doses can escalate for each infusion up to 1 mg/kg over 40 minutes.
We will generally have you wear a scopolamine patch and take Ondansetron prior to arrival. We offer an array of medications to keep comfort to a maximum should you feel nauseated or anxious.
Patients have described the infusion on a number of levels. Many describe initially feeling numbness and tingling, heaviness, and a sense of relaxation initially.
The Empathogenic experience of ketamine includes a sense of body awareness, reduced ego defenses, empathy, warmth, love, and peace. For others, euphoria and a dreamy state are pronounced emotional states.
Out of body experiences occur at higher doses, in which one feels a departure from their body, loss of identity, an experience of being a single point of consciousness, or even mind-death (psychological death). Others may feel they are part of a collective consciousness and have transcended normal time and space or being at unity with nature and the universe.
Ketamine offers a shift in the usual ways of being and viewing oneself and the world. It is effectively a time-out from your ordinary mind. Ketamine infusions offer relief from depression and a reset for new consciousness. The relief of depression is accompanied by a relief of negativity.
The Recovery Process
We will closely monitor you throughout the IV infusion process. You will be attached to our monitors and our infusion team will ensure that you are safe until the treatment is complete. After the procedure, you will stay in your room until you feel comfortable, and the medical staff has evaluated you for safe discharge. The main side effects are dizziness, nausea, and balance control issues that resolve within one to two hours. Driving is not permitted for four hours.
When Can I return to work?
Many patients will work the next day or even several hours after their infusion. The dissociative and mind-altering effects are gone within 20 minutes after an infusion. Any good feelings or changes you notice the next day or later that day are due to the neuroplasticity of ketamine. Again, driving is prohibited for four hours. You otherwise will be fully functional in between infusions.
How Often Can I receive Ketamine Infusions after my series of infusions?
We recommend every 2-4 weeks that you receive a booster infusion. If symptoms worsen, you can return more frequently.
How Does Ketamine Help Depression?
Unlike classic antidepressants, ketamine affects the nerve signaling that occurs via the glutamate system and results in the production of Brain Derived neurotrophic Factor (BDNF) with subsequent neuroplasticity, neural circuit repair, synapse formation, and calming of the anxiety centers of the brain (the amygdala) When the medicine has an effect, it relieves depressive symptoms and suicidal thoughts very quickly.
What Are The Different Types of Depression?
Depression is a debilitating mental disorder that brings feelings of intense sadness and isolation. According to NIMH (The National Institute of Mental Health), somewhere around 16 million American adults suffer from at least one major depressive episode in any given year.
Unfortunately, many suffering from depression feel incredibly isolated and decide not to seek treatment. While depression usually can not be “cured” with treatment, the symptoms can be managed.
Depression itself varies greatly from case to case. Some people may suffer from persistent depression, while others may only get it temporarily or episodically. There is a litany of different versions of depression, each with their own symptoms and triggers.
Some of the typical diagnoses of depressive disorders may include:
Major Depressive Disorder (MDD):
Also known as clinical depression or unipolar depression. The most common form of depression. It can be just a single episode, but some people may experience it periodically throughout their lives.
Postpartum Depression:
A type of depression usually brought on by the hormonal shifts women experience the months or year following childbirth.
Seasonal Affective Disorder (SAD):
This type of depression is caused by a change in the circadian rhythm of the body, usually bringing on depression during a specific season of the year.
Situational Depression:
While the symptoms are much like major depressive disorder, this is depression brought on by a specific event, such as the death of a loved one or a life-threatening event.
Persistent Depression:
Also known as dysthymia or chronic depression, this is depression that can affect sufferers for two years or more.
Manic Depression/Bipolar Disorder:
Characterized by periods of mania alternating with periods of intense depression.
What Are The Symptoms of Depression?
Those suffering from depression will have trouble functioning in their daily life and may fall behind at work or school. Depression may also affect personal relationships and physical health. That said, the symptoms of depression can sometimes be greatly different between different cases.
The common symptoms include, but are not limited to:
- Sadness or melancholy
- Hopelessness
- Anxiety
- Loss of interest in hobbies
- Change in eating or sleeping patterns
- Trouble concentrating
- Fatigue or lack of energy
Depression also has a risk factor for developing other problems, such as higher rates of chronic disease. Depression tends to also bring an increased risk of both blood clots and more general heart disease. Some may even turn to substance abuse in an attempt to alleviate the symptoms of depression.
What Is Clinical Depression?
Clinical depression sometimes referred to as major depressive disorder, is usually diagnosed when someone is suffering from depression that has persisted for two weeks or more and experiences the symptoms throughout most of the day.
Usually marked by disinterest in hobbies and persistent sadness, which then leads to negative changes in diet, concentration, hygiene, and overall behavior.
Millions of people suffer from depression every year. You should feel no shame in deciding to find treatment.
Symptoms of Clinical Depression
- Fatigue
- Changes in sleep pattern
- Weight fluctuations
- Mental fog
- Agitation
- Loss of sexual interest
What Causes Clinical Depression?
Genetics:
Clinical depression can pass through genetics from relatives who also suffered from depression.
Brain Signals:
Neurotransmitters within the brain may not be responding to how they should. This miscommunication causes feelings of depression to intensify.
Chemical Imbalances:
Research shows that the chemical structure of the brain is wired differently in those with clinical depression.
Hormonal Irregularities:
Clinical depression is sometimes triggered by the hormones in the body is unbalanced. Some bodily changes (like pregnancy, thyroid problems, or menopause) may be responsible for these irregularities.
Sorry. We don’t accept insurance, but we can provide you with a SuperBill, which is a statement to provide to your insurer for compensation.
What recovery services do you offer?
We treat patients with opioid and alcohol addictions by providing multiple interventions. Included are Suboxone, Sublocade, Probuphine, and Naltrexone (Vivitrol) support for opioid addictions. We offer standard therapies for alcohol disorders which include Antabuse, acamprosate, and naltrexone. We offer the Sinclair method for decreasing alcohol use. We also use off-label treatments , including Topiramate, baclofen, and gabapentin therapies to help with the cravings and withdrawal symptoms. Call for an appointment or questions regarding treatment costs. We also offer progressive outpatient detox therapies for opioid disorders, which includes Lucemyra therapies, which allows you to be more comfortable during detox.
Do you offer ketamine for depression and other mood disorders?
Yes. Ketamine is used off label as a rapid acting anti-depressant and has been effective in patients with resistant depression, bipolar disorder, PTSD, fibromyalgia, and anxiety disorders. The protocol varies depending on the underlying condition, but the procedure takes place in a comfortable, monitored setting in our office. You can call 703-854-9608 to discuss details and questions with the staff. Insurance generally does not cover the treatment, but we can provide a superbill as well.
Do you offer IV vitamin therapies for nutritional deficiencies?
Yes, we use progressive IV therapies designed individually for each patient based on their nutritional lab studies. Multi-minerals, zinc, B vitamins, high-dose vitamin C, Magnesium, and others are frequently combined to provide a nutritional replacement to pre-operative, post-operative, depressed, or generally-ill patients. These formulas may give that extra energy and wellness to those with conditions such as fibromyalgia, cancer, addictions, alcoholism, and many other medical conditions. Contact us today for an evaluation. For more information, check out IV vitamin center.
Ketamine has been shown to stimulate neuron growth in the brain in as quickly as one hour. Many scientists studying ketamine are focusing on the neurotransmitter glutamate, which plays an important role in neural activation.
What’s involved in the ketamine infusion process?
Patients will receive infusion therapy in a private room with constant mechanical monitoring of heart rate, pulse, blood oxygen saturation percentages and blood pressure. Infusion therapy means an IV will be placed and an appropriate dose of ketamine will be administered over a 40 min time frame or longer. Practitioners are able to see a patients vital signs from the monitors at all times from the nursing station. However, patients will notice that a practitioner will enter the patient treatment room several times during the active phase of the infusion to monitor the depth of sedation and ensure patient comfort. Most patients report a relaxing and peaceful experience. Patients will most likely experience changes in vision and their ability to clearly focus on objects or people, speech will be slurred or slowed, most will have an experience of floating or being disconnected. Patients on average should expect to spend 90 to 120 minutes in the office allowing for the check in procedure, the active phase of infusion and recovery time. Patients will need a trusted friend or family member to drive you home after your infusion. Patients may drive and return to work the next day. Patients may have a friend or family member in the treatment room during infusion, but this is not necessary.
Is ketamine dangerous or ineffective?
Ketamine is a very safe medication – it has been used since 1970 for anesthesia and is on the World health Organization’s list of Needed medications since 1986.
What is the process for a ketamine treatment?
Most patients report significant improvement by the (3rd) third infusion and more than 80% report remission at the (4th) infusion. In addition, there are some patients that initially become aware of improvement in mood and well-being through loved ones such as a spouse, and this can occur after only one (1) infusion. Some patients want further gains before moving into maintenance and will continue to receive infusions at a frequency of two infusions per week until they reach remission or improvement levels they deem satisfactory. Typically this is achieved by the (6th) sixth infusion. Nova Health Recovery follows empirically proven protocols for loading dosages; 4 to 6 infusions delivered at a frequency of twice per week for 2 to 3 weeks. Once patients complete this loading dose protocol they begin the maintenance phase of treatment which is highly patient-specific. As a general rule, patients can expect to return for maintenance infusions about every 4 weeks for the first 12 months following treatment onset. At Nova Health Recovery, we are seeing the effects of treatment as more durable over time, meaning patients appear to maintain results over longer periods of time and require fewer maintenance infusions after 12 months in the maintenance phase.
What is the ketamine success rate?
Approximately 70-80% of patients respond to ketamine infusions.
How Is Ketamine Therapy Administered?
Rapid treatment for mood and painful disorders is generally imitated with IV Ketamine. This works the fastest and insures steady-state levels in the blood stream. There are also nebulized, intranasal, and oral troche ketamine forms as well. We generally use intranasal and troche (lozenges) forms of Ketamine as initial or add-on therapy for depression, PTSD, and other conditions.
How Many Sessions of Ketamine Infusions Will I Need?
It depends on the condition and severity of illness. Generally for depression, a series of 6 infusions over 2-3 weeks is recommended for maximum impact. We recommend not more that 6 days apart. PTSD may require only two sessions a week apart. CRPS pain protocols require multi-hour infusions several days in a row.
How Rapid Does Ketamine Work For Depression?
Ketamine results are seen by the third infusion in those who respond. For those with response, the infusions may need to be repeated as a single infusion in the following sessions at any time after the series is completed. Some patients will notice improved mood the day after an infusion, yet for other, it may take a few infusions to start to break the depression cycle.
What is the Response Rate to Ketamine Infusion for Treatment Resistant Depression?
70% of all treatment resistant patients have a 50% improvement in their depression scores ( We use the Beck Depression Inventory and PHQ 9 to measure depression. ) We see many anxiety patient having slightly less improvement but still significant recovery.
How Long Do the effects of Ketamine Last for depression therapy?
This varies for each person. For some, the effects last for months, while for others, monthly or quarterly infusions may be needed to continue the effects. We utilize a home-based ketamine spray to help maintain the benefits of the infusions and avoid repeat infusions. Most patients should expect to have the need for an infusion every 2-3 months. This may seem like a lot, but if you feel awesome, the value of the treatment is priceless.
Is Ketamine Safe ?
The safety window for Ketamine is incredibly high – there is minimal risk with the dosing used in therapies for depression and anxiety. The main possible side effects include spasmodic bladder issues, elevated liver enzymes, dizziness, and nausea. Repeated Ketamine infusions have been shown to be safe.
Is Ketamine Addictive?
In Asian populations, Ketamine has been misused in the context of raves. There may be a preference to use the drug, but there is no withdrawal when one stops using it. True addiction to Ketamine is rare.
What does the Ketamine Infusion Feel Like?
Ketamine infusions vary from each infusion, with some being pleasant while others may be anxiety-provoking or sad. With re-direction or guided imagery, the infusion may be assisted in achieving goals of mindfulness or resolving an internal struggle. The main side effects of dizziness and nausea are prevented by the administration of Zofran prior to the infusion. Many patients are awake during the treatment, listening to ambient, soothing music that helps guide their visions. The infusion can be stopped at any time and the feelings go away within minutes. In general, most find the infusion to be amazingly pleasant and mood-lifting.
Can I start treatment with the Ketamine nasal spray?
Yes. The home-based nasal spray is effective as well, but not as rapidly as the infusions. The home-based ketamine spray is compounded in specialty pharmacies and the dosing pattern is determined by your condition. We use the spray or troches for the same conditions as the infusions. The spray works well in those with a fear of needle sticks. We do a consultation for both the spray or infusion to determine appropriateness. We use the nasal spray starting around the fifth infusion and thereafter to consolidate the gains from the infusion.
Does Insurance Cover Ketamine Infusions?
No, but some will cover some out of network expenses. This is generally done through a superbill in which the physician will outline the codes for the procedure that was done so it can be submitted for compensation. We do accept CareCredit, which is a medical credit card with 6 or 12 month interest free options.
How Much is A Ketamine Infusion?
Each infusion costs $480 and lasts for about 50 minutes I tell everyone to expect a 2-hour total time in the office. Remember you cannot drive for 6 hours after the use of the Ketamine. Infusions for CRPS last about 4 hours and cost around $1600. The consultation fee prior to the infusions are $350.
What other therapies are available for depression and Anxiety treatment?
We also utilize dextromethorphan therapy and scopolamine for depression and anxiety treatment. They are both highly effective. They behave as a rapid depression reversal agents, with dextromethorphan acting on the NMDA receptor, whereas the scopolamine, given IV or oral, works on the cholinergic system. We also use nutritional supplements to add into your treatment.
What disqualifies me from Ketamine Treatments?
Allergies to Ketamine, active heart disease and liver disease prevent us from treating individuals with Ketamine. Also, if there is a history of psychosis or schizophrenia , then Ketamine should not be used. Ketamine works less well once you are over 50 years old as the depression and mood may be a result of early dementia in some individuals. Neuropsychiatric testing works well to evaluate this. We still use Ketamine in patients as old as 90 years old and as young as 15.
Can adolescent patients receive Ketamine?
Yes, we infuse children as young as 15 with excellent results. Ketamine is very helpful in perimenstrual dysphoria and dysmenorrhea.
A few notes:
Ketamine works at the neuroplasticity level in the brain, ramping up the reward pathways and down-regulating anti-reward pathways. It cannot change your personality or your boss or significant other. External stressors don’t respond to medication and will still be there after the therapy, however, with a better mood, your coping skills will improve dramatically.
How do I get started with Ketamine therapy?
That is the easy part: just call 703-844-0184 and make an appointment, or email us below. We have immediate appointments available and No Referral is needed.
Depression is a leading cause of disability worldwide.
Depression changes the function and structure of the brain. There are neurochemical, neuroendocrine, and anatomical changes that occur.
Neurochemical Changes:
Neurotransmitter abnormalities of serotonin, noradrenaline, and dopamine (monoamines) have been found in depression. Examples of neurotransmitter aberrations have been found with the serotonin transporters in the midbrain and amygdala (fear/emotion center) as well as with decreased 5-HT1A receptors in the frontal and limbic areas of the brain. These changes stay present in patients even after depression resolves.
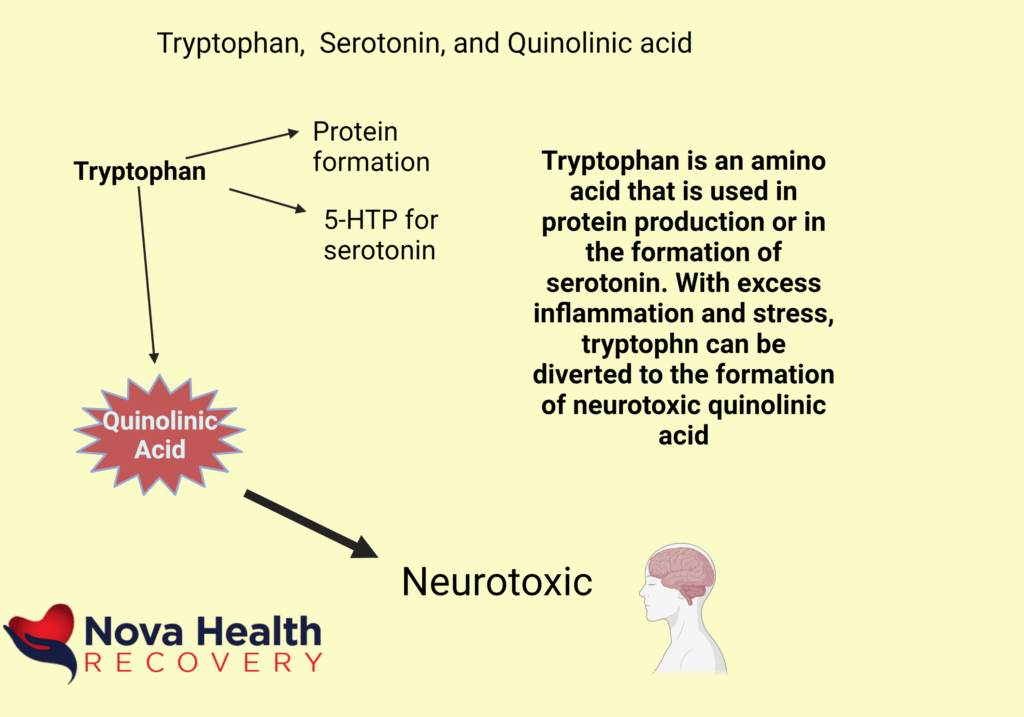
Other systems and neurotransmitters are involved with depression. It has been found that depriving individuals of tryptophan, which is involved in the production of serotonin, does not result in depression in every patient, but sometimes in those with a history of depression.
The GABA system and the Glutamate system also are also associated with depression. Glutamate is a key system involved in mood disorders.
-
There is decreased density of GABA interneurons in certain areas of the brain in depressed patients. These areas include the prefrontal cortex (executive functioning center) and the occipital areas of the brain.
-
-
There is lower GABA levels in the spinal fluid of depressed patients as well.
-
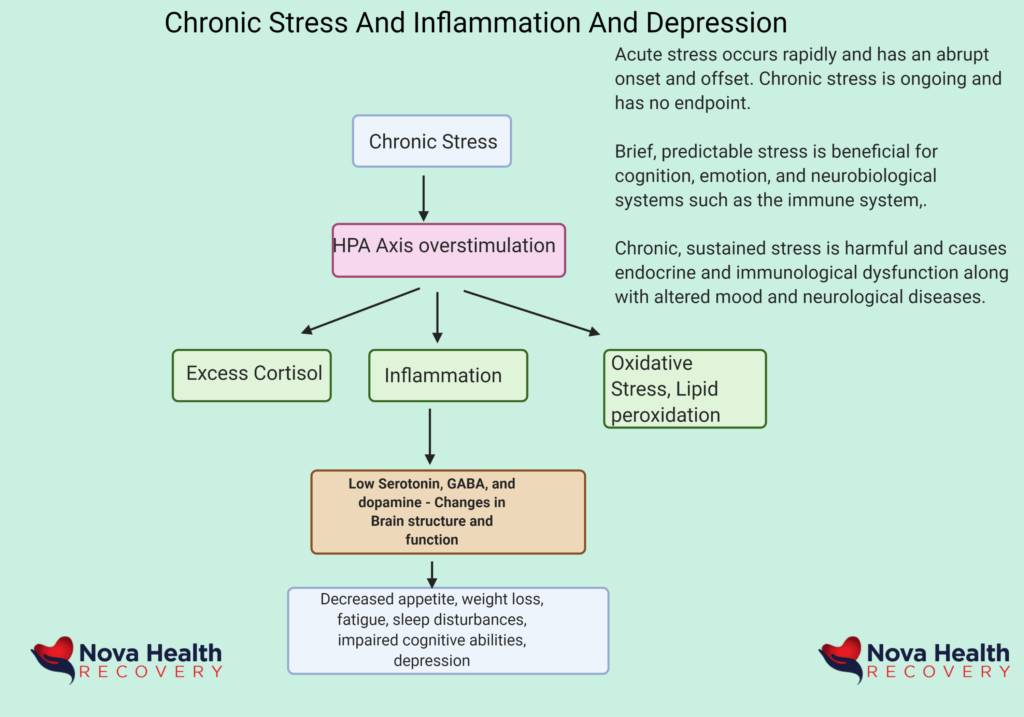
Neuroendocrine changes are also found in depression. This can be seen in Cushing’s disease, in which depressive symptoms can be high. Elevated levels of cortisol produce depression. Elevated 24-hour cortisol, increased waking salivary cortisol levels, and elevated 24-hour cortisol blood levels are all associated with depression. Long-term exposure to elevated cortisol results in cognitive impairment and volume reductions in an area of the brain involved in working memory, the hippocampus. There are frequent comorbidities associated with this such as diabetes and heart disease as well.
Early life stress is associated with hyperactivity of the HPA axis as well later in life. This can result in cortisol excess and depression. Elevated salivary cortisol is also seen in patients at risk of depression as well.
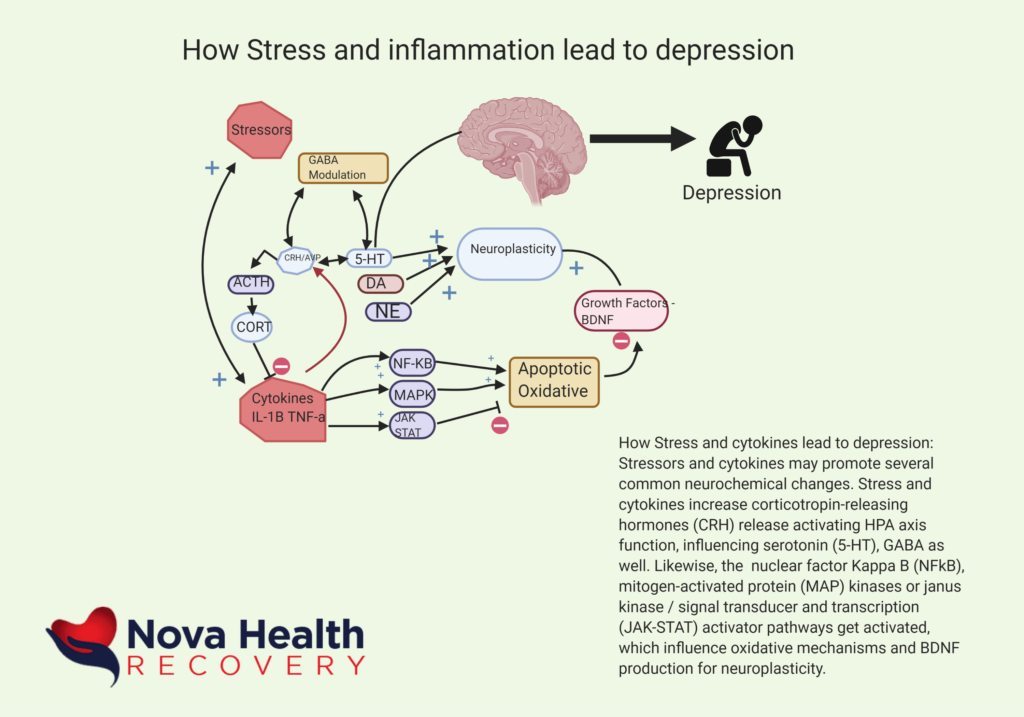
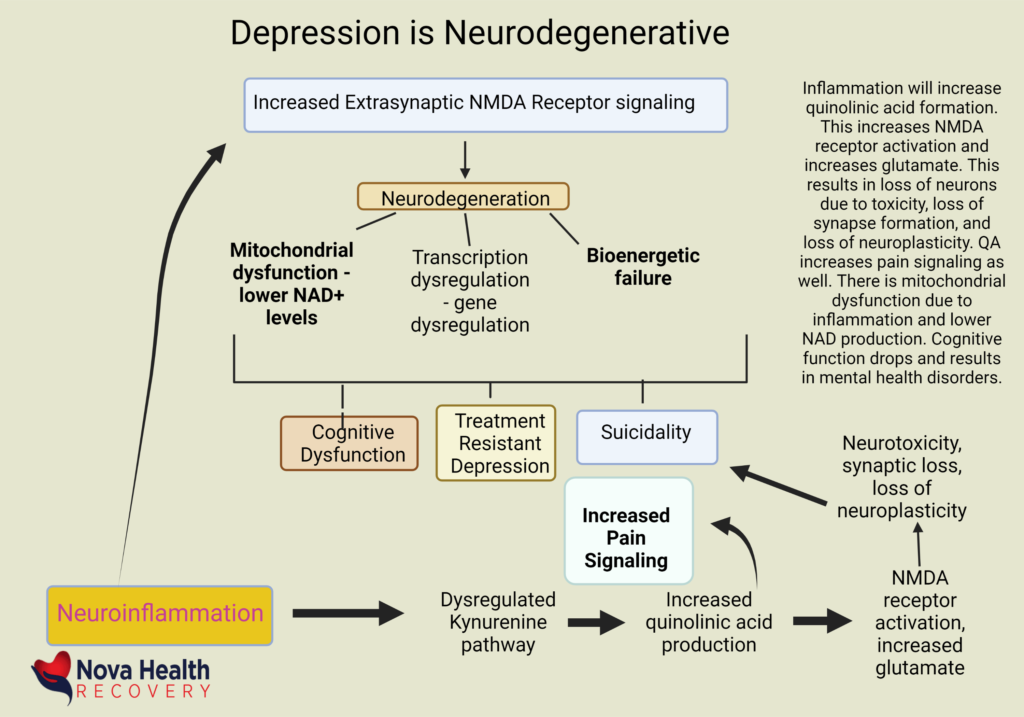
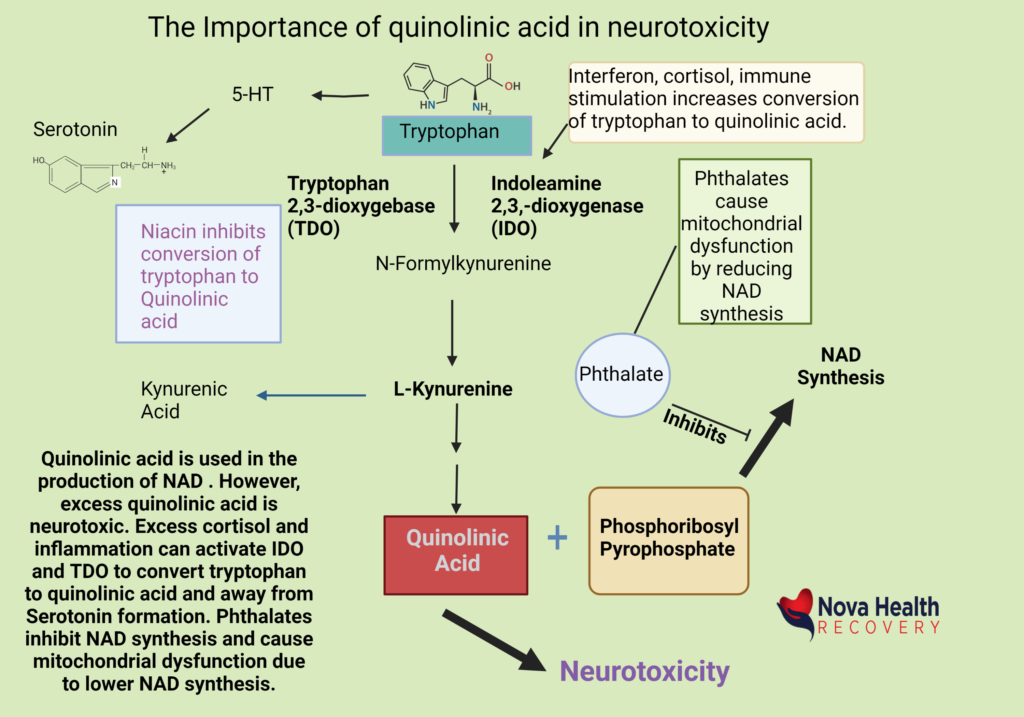
Finally, inflammation may play a role in depression as increased biomarkers such as C-reactive protein (CRP), interleukin-6, and tumor necrosis factor alpha al found to be associated with worsened depression. The use of interferon-alpha, for example, is associated with the production of depression in normal individuals. This may be due to the production of quinolinic acid from the degradation of tryptophan. Inflammation causes the activation of indoleamine 2,3-dioxygenase, which increases the shunting of tryptophan into quinolinic acid. Quinolinic acid is neurotoxic and increases the risk of depression. There is evidence that treatment with anti-inflammatories may decrease depression.
Structural changes in depression:
Some key areas affected in depression include:
-
The orbitofrontal cortex
-
Basal ganglia
-
Hippocampus
-
Amygdala
-
Anterior cingulate cortex
-
Grey and white matter changes are seen in depression:
-
Decreased hippocampus volumes (working memory center)
-
Decreased size of the prefrontal cortex (executive decision-making)
-
Anterior cingulate cortex (subgenual)
There are multiple potential causes of volume loss , and this includes decreased synaptic connections and glial cell and neuronal cell death. White matter lesions also occur in depression with increasing white matter lesions and are felt to interrupt limbic projections to the frontal cortex. These are associated with increased apathy, depression, and psychomotor retardation.
There are also blood flow changes noted in depression as evaluated with single-photon emission tomography (SPET), positron emission tomography (PET) or functional magnetic resonance imaging (fMRI). Areas with altered and lower blood flow include the anterior cingulate cortex, the prefrontal cortex, and amygdala.
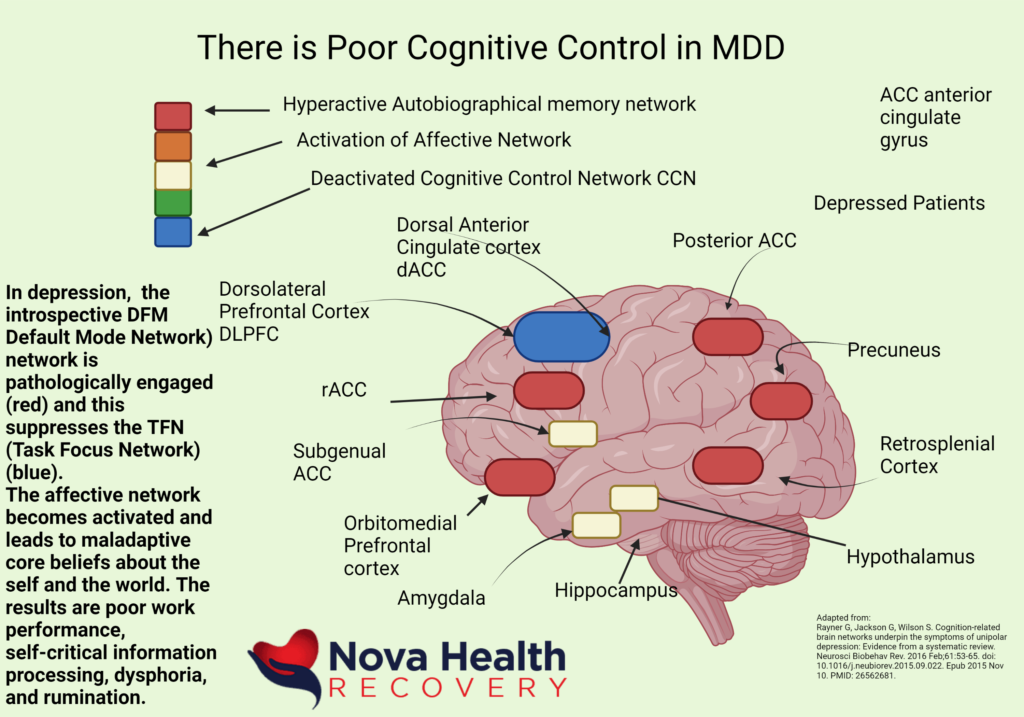
Functional connection changes are also seen in depression. In other words, the networks of the brain are impacted in depression such as the cognitive control network, the default mode network, salience network, and the affective network can be altered in depression. Increased resting state functional connectivity is seen in depression in the affective network. In the default mode network, there is increased task-related activity as well. This causes the person to be less ‘in the moment’ and the individual tends to daydream more and feel more anxious.
Impaired Cognition in Depression:
There are issues in processing of information in depressed individuals and in dysfunctional attitudes noted in patients with mood disorders.
Abnormalities of cognitive domains in depression include:
- Perception
- Attention
- Memory
Cognitive issues in depression include those involving emotional content (hot) and those not associated with emotional content (cold) .
|
Hot Cognitive Impairment |
|
|
Attention |
Impaired processing of reward |
|
Impaired processing of punishment-related experiences |
|
|
Memory |
Poor processing of emotional stimuli |
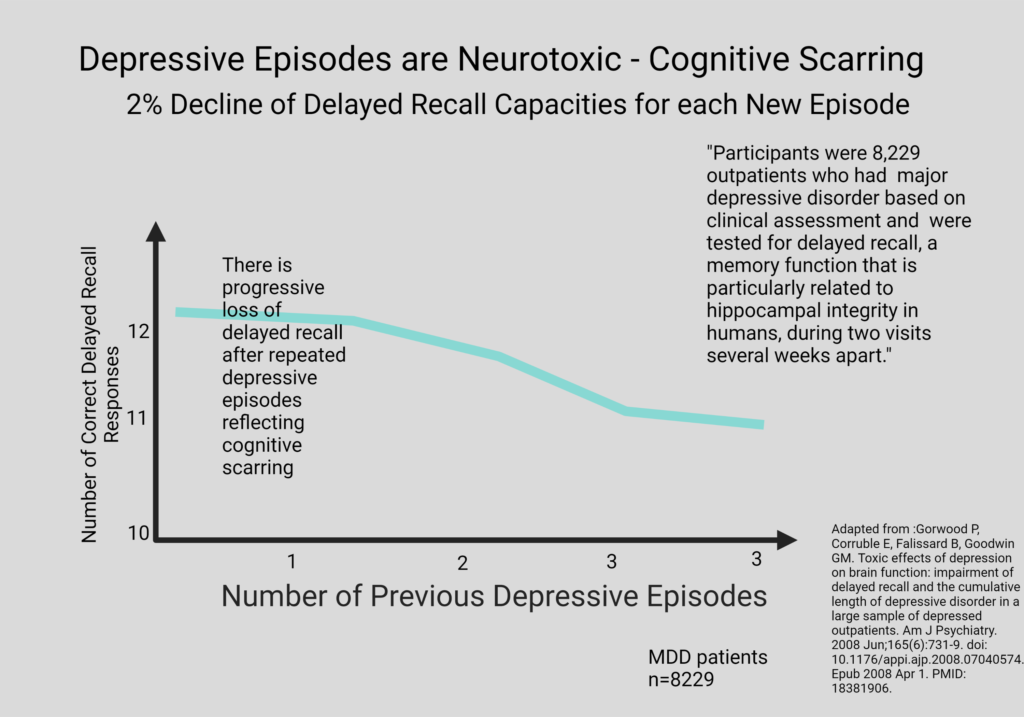
The cognitive impairments in attention, executive functioning, and memory tend to occur in more severe depression and in those with chronic courses. They respond poorly to treatment.
Cognitive abnormalities associated with mood that are emotional in nature tend to focus on negative biases and impaired reward processing or punishment-related experiences in depressed individuals. Persons who are at risk for depression also have difficulty in processing emotional information as well. For example, depressed individuals have difficulty processing negative feedback relative to non-depressed peers. Likewise, there are difficulties in the processing of positive feedback in depressed patients as well. For a depressed person, the glass will always feel ‘half-full.’
Depressed individuals also demonstrate impaired motivation for specific effort-related tasks.
The Neurobiology of depression is a multifactorial disorder.
- Recurrent depressive episodes may result in enduring functional and structural alterations in critical brain areas.
- Disruption in corticolimbic circuits of the brain creates neuroendocrine, neuroimmune, and sympathetic dysregulation.
- There is inadequate monoaminergic and neurotrophic signaling in depression with excessive glutaminergic and inflammatory cytokine transmission. This causes glial-neuron breakdown, which further impacts corticolimbic processing.
- The brain has neurotransmitters and mediators such as CRH and GABA and others that are involved in stress responses and modulation. The role of inflammation in this process is important. It also has resilience units within it such that they respond to acute stress, but the impact of constant stress alters Brain derived neurotrophic factor (BDNF) and results in functional distress in the brain.
Reward processing errors and motivational deficiencies are a clear part of depression and anhedonia. In depression, there are cognitive biases and difficulties in processing positive or negative feedback. Individuals with depression have difficulties functioning in societal contexts which require focus, concentration, and constant feedback. They will always view a neutral interaction or facial expression as being a negative one, hence the low self-esteem, self-sabotage, and ruminations.
What is the Wiring in the brain involved in depression?
Here are some basic contexts of cognition and emotion as related to brain structures:
Hippocampus: Memory and feedback to the HPA
Amygdala: Memory of emotional reactions
Anterior Cingulate Cortex: Reward anticipation, empathy, emotion
Orbitofrontal cortex: Social interaction, maternal behavior
Prefrontal cortex: decision-making, planning, and judgement
The disruption of functional and structural neural circuits underlies the dysregulation of mood and function in depression. Sustained stress can disrupt neural activity in circuits of the brain.
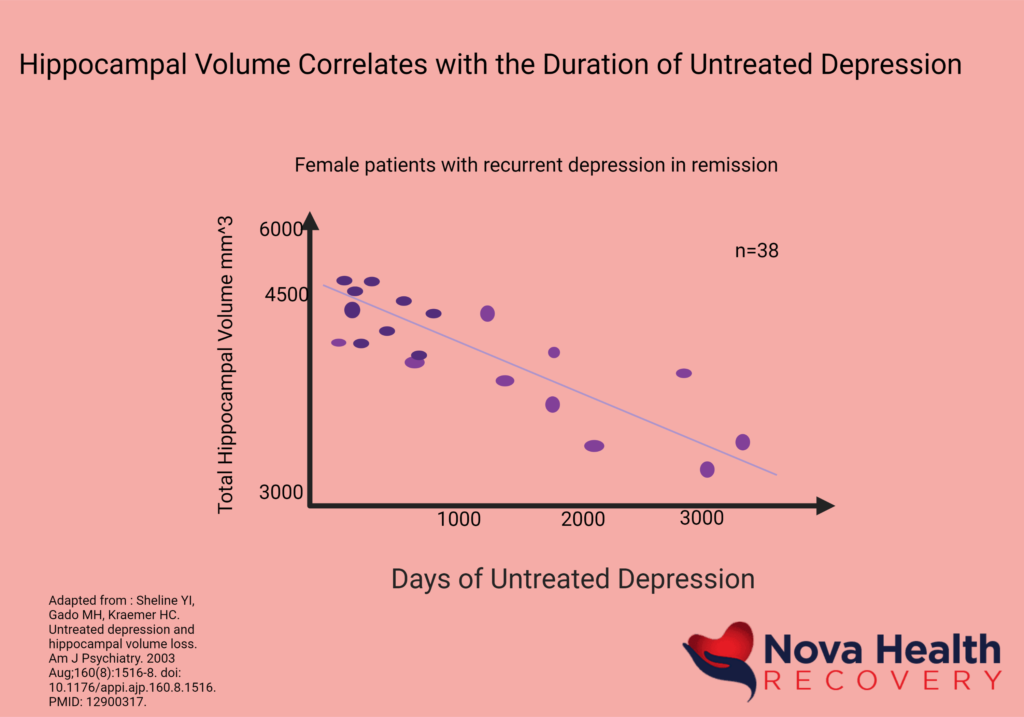
The neuronal activity of the brain follows the blood flow and can be monitored in depression. There is increased blood flow to the amygdala and ventrolateral PFC (prefrontal cortex – both left medial and lateral orbital cortex) in depressive disorders. There is increased amygdala activation in depression as well as ventrolateral and medial areas of the prefrontal cortex. Increased amygdala metabolism is associated with elevated plasma cortisol level and this is seen in depression. Thus central, dysphoric activation is associated with hypercortisolemia and systemic responses as well. This blood pressure goes up and insulin metabolism changes with increased insulin resistance, changes in pain perception, decreased quality of sleep all occur with increased depression and stress. If sustained stress activation occurs over weeks to months, depression changes the structure and function of the subgenual anterior cingulate gyrus. The brain shows reduction in volume, neuronal loss, and also loss of richness of cell environment in key regions such as the subgenual anterior cingulate gyrus, which is involved in anticipation, planning, and pursuit of life’s pleasures. Likewise, hippocampus volume decreases, which affects working memory. In other words, untreated stress and depression results in volume loss of key brain regions such as the hippocampus.
- Compared to normal controls, depressed patients had smaller hippocampal volumes
- Decreased hippocampal volume may be related to the duration of depression.
- Therefore, we need to prevent subsequent episodes of depression as it promotes successive damage.
- The size of the hippocampus is related to the number of untreated days of depression. The longer you remained depressed, the smaller the hippocampus becomes! If treated, there is no hippocampal volume loss.
- Greater activity and volume of the anterior cingulate (ACC)may be associated with faster treatment response in depression. In other words, patients with greater subgenual ACC volume had faster improvement and fewer residual depressive symptoms with treatment.
- Resilience, neurogenesis, and synaptogenesis play roles in depression. The neurobiological effects of depression extend beyond the monoamine pathways.
Inflammation plays a role in many cases of depression. In fact, elevations of the inflammatory marker C-reactive protein (CRP) made in the liver and IL-6 are associated with increased risks of depression. In fact, the injection of the inflammatory agent interferon-alpha, historically used in the treatment of hepatitis, is associated with depression in 50% of patients injected with this medication and sickness behaviors such as fatigue and malaise in 90%. Psychological and physical stress results in the release of inflammatory mediators that in some individuals who release large amounts of inflammatory cytokines results in depression at a higher rate. Stress increases cortisol levels through corticotrophin releasing hormone and this causes increased gut permeability with enhances inflammation as well as endotoxin from the gut permeates through the intestine.
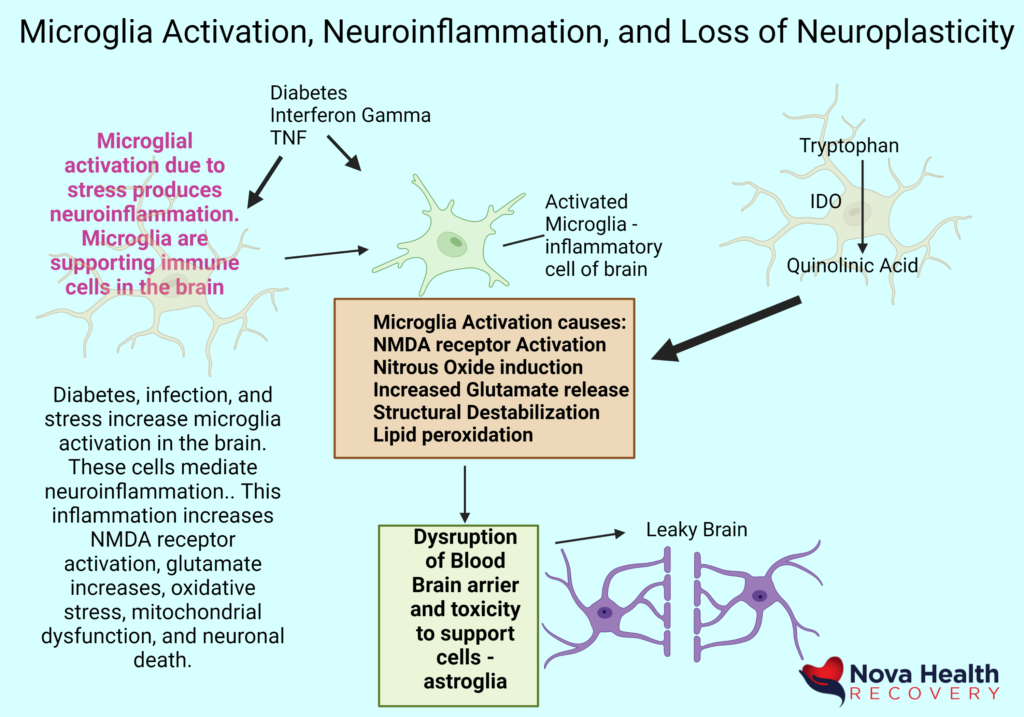
Obesity also increases general inflammation and produces an increased risk of depression as well as a worsened metabolic profile. The inflammation has a bidirectional flow with the nervous system and results in neuroinflammation and resultant depression. Inflammation also causes tryptophan to be shunted to the production of Kynurenine and Quinolinic acid, which are NMDA receptor agonists and are neurotoxic. This results in lower serotonin levels as an enzyme 2,3-dioxygenase (IDO) becomes activated to shunt tryptophan from serotonin. Stress and infection will shunt tryptophan by activation of the IDO enzyme thus lowering serotonin levels and producing depression. The increased levels of kynurenine can be improved through exercise, which can activate an enzyme in muscle known as KAT (Kynurenine aminotransferase) which converts kynurenine into kynurenic acid, which is not toxic). Increased inflammation in the brain as well as increased levels of kynurenine and quinolinic acid also reduction in dopamine, the molecule of reward. Thus, in states of inflammation with increased kynurenine and quinolinic acid, lower dopamine and serotonin is found, causing the person to not feel rewarded with the basic things in life. This is also explains the anhedonia resulting from inflammation, infections, and medical illness.
How to calm the inflammation in depression:
Omega 3 fatty acids can decrease inflammatory responses in the brain and improve mood. Eicosapentaenoic acid and docosahexaenoic acid, omega-3 fatty acids that are found in fatty fish and fish oil supplements, promote the production of anti-inflammatory mediators such as resolvins and protectins. One trial demonstrated reduced depression in individuals supplemented with omega-3 fatty acids, in particular EPA. Similar findings of the antidepressant effect of omega-3 fatty acids on depression have been seen in other studies as well, even augmenting the effect of traditional antidepressants as well. A meta-analysis of omega-three fatty acids demonstrated EPA supplementation to be effective in reducing depression.
Exercise also offers benefits as an anti-inflammatory treatment of depression. It has been shown that inflammation occurs every time we eat and exercise may be a way to diminish this response as well as chronic inflammation.
Whole Body Hyperthermia also represents a way to improve mood in depression. Exposure to cutaneous heating (41°C) activates the midorbitofrontal cortex, the pregenual anterior cingulate cortex, and the ventral striatum, with the degree of activation being associated with subjective pleasantness ratings made in response to the warm temperature. Patients with MDD display abnormalities in thermoregulation characterized by increased core body temperature and reduced ability to sweat, both of which have been reported to normalize following successful treatment. Effects can be seen for up to 6 weeks. The mechanisms of this treatment may involve heat shock proteins and the increase of BDNF which increases neuroplasticity.
Sauna use
Sauna use reduces depression through heat shock proteins and pro- and anti-inflammatory factors, which in studies, demonstrated improved depression, improved appetite, reduced body aches, and anxiety. Elevating the core body temperature up to 101.3 F also has an anti-depressant effect that can last up to 6 weeks in another study.
Bright Light Therapy
Circadian disruption is common in depression and our circadian rhythm modulates our hormones, hunger, metabolism, and numerous processes based on a 24 hour cycle with many of our genes (10-40%) being linked to the circadian cycle. External cues such as external lights and food can disrupt the cycle if we are exposed at the wrong time to them as frequently happens in nightshift work or during travel. This can disrupt the production of melatonin, which is involved in the preparation of the body for nighttime as well as enhancing mood. In Seasonal Affective Disorder, melatonin replacement can be a helpful treatment for depression. The key to a healthy circadian system is to not eat beyond 7 P.M. and also avoid blue-light/screens in the evenings.
Cortisol elevation also is associated with depression. This can be impacted by exposure to bright light therapy (10000 Lux) , which can also treat non-seasonal depressive disorder. Blue light improves mood and boosts alertness in early daytime hours, with cortisol levels being reduced with 10000 Lux exposure in one study. Sleep is generally poor in depression and can trigger suicidal ideation. Bright lights at night can trigger melanopsin release which can alter the brain’s internal clock, the suprachiasmatic nucleus, and can shift the brain into a daytime pattern, resulting in insomnia.
Mindful meditation also has a positive impact on mood and depression. Mindfulness is a way to improve attentional skills and places one into a flow state. An MRI study demonstrated the decrease of the amygdala’s activation in stress after mindful meditation. Emotional regulation can be enhanced by doing this practice. Studies have shown that people with moderate stress who practice mindful meditation had greater improvements in depression relative to those who received only basic health education. Mindful meditation also reduces anxiety, depression, and pain based on the results of a meta-analysis of 47 studies.
Transcranial Direct Stimulation (TDCS)also provides a way to diminish depression by applying scalp electrodes to a portable battery-powered generator which results in modulation of the local neuronal circuits and alters synaptic transmissions, allowing them to change their strength. TDCS also improves depression symptoms beyond one month of treatment relative to SSRI’s in one study. The ability to read emotions such as disgust, anger, and happiness on other’s faces is impaired in depression but is improved with TDCS per another study.
Probiotic Use for depression:
Fermented foods and dietary supplements can aid in mental health – fermented foods like Kimchi and sauerkraut may be helpful, but one study with 2.5 billion bacteria per gram of Bifidobacterium bifidum W23, Bifidobacterium lactis W52, Lactobacillus acidophilus W37, Lactobacillus brevis W63, Lactobacillus casei W56, Lactobacillus salivarius W24, and Lactococcus lactis (W19 and W58) for four weeks demonstrated improved mood and less ruminations.
Dietary Impact on Depression:
Depressed individuals are frequently deficient in key nutrients that are involved in neurogenesis and inflammation such as folate, Vitamin B6, Vitamin B12, and Omega-3 Fatty acids and in one study in Spain, depression was increased in persons with these deficiencies.
Fresh fruits, vegetables, fatty fish, and a Mediterranean diet is associated with improvement of depressive symptoms. The “Smiles” trial demonstrated that dietary adjustments could improve depression outcomes. The modification of diet and lifestyle in obesity and depression demonstrated food interventions to diminish depression in another study and also in other interventions of dietary and behavioral changes in obese and depressed patients. A wide variety of fruits and vegetables has increased phytonutrients such as stilbenes and isothiocyanates which provide a hormesis to benefit stress response pathways to reduce inflammation. Critical vitamins such as Vitamin C, folate, and B complex, as well as magnesium, zinc, and molybdenum are also improved in such a wide-ranging diet. These nutrients and vitamins are involved in the production of neurotransmitters and proteins to improve depression.
Brain Inflammation and microglia
Some individuals have an increased propensity to concussion, trauma, and ultimately cognitive decline from neurodegeneration, a syndrome called Diminished Brain Resilience (DBR) syndrome:
There is an increase in TBI (traumatic brain injury) which is not due to increased sports activity. This is due to increased vulnerability to mild trauma, which also increases the risk of chronic pain and depression. This is related to neuroinflammation.
Inflammation can represent a lot of different things, such as inflammation of mucus membranes in the nose from allergies, or damage from an injury with inflammation and swelling due to infection. The mechanisms here are different, one being caused by histamine response and the other being due to infection with swelling, redness, and all the signs of inflammation.
Chronic central sensitization represents neuroinflammation and correlates to:
- Anxiety disorders
- Chronic back pain
- Chronic migraines
- Fibromyalgia
- PTSD
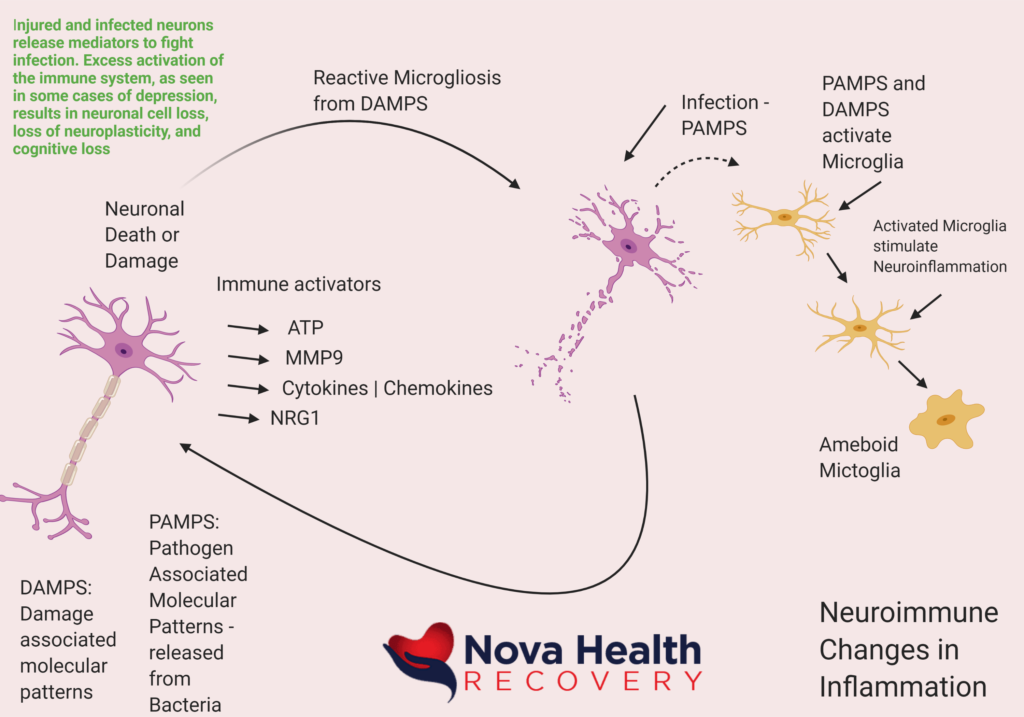
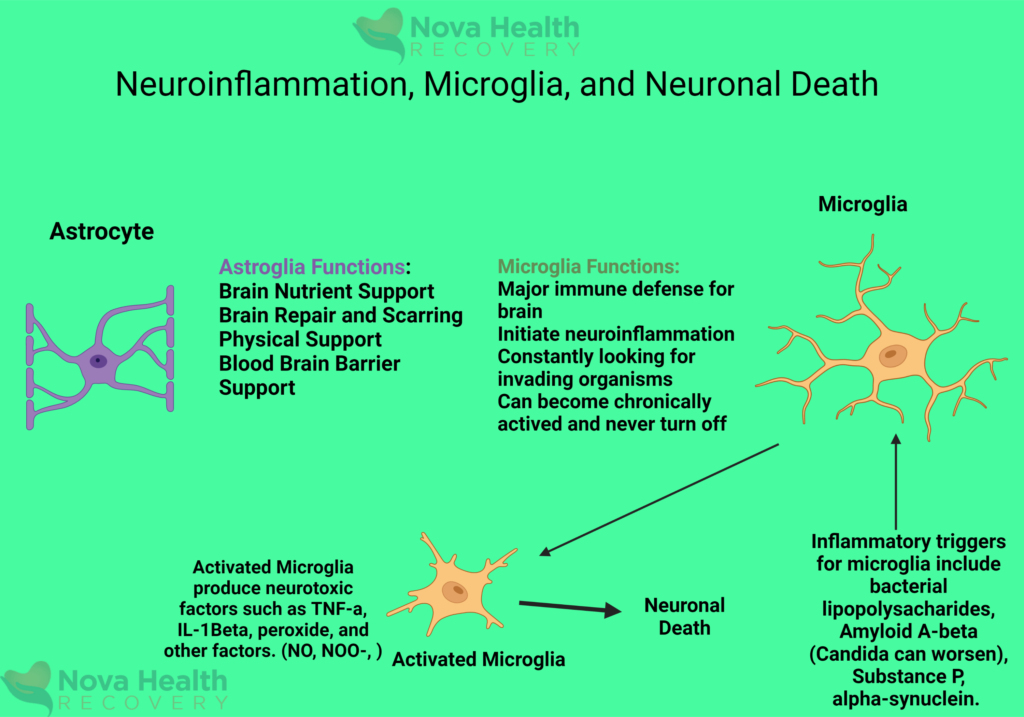
When neurons die due to trauma, infection, and inflammation will cause the release of chemokines, ATP, cytokines, and other immune activators. These cause repair mechanisms to activate and try to prevent further damage. These activated microglia can transform into an inflammatory state and send out inflammatory compounds which can destroy other neurons.
In the event of injury or infection, brain cells release various mediators:
DAMPS : Damage associated molecular patterns – are released from dying cells as found in concussion injuries
PAMPS: Pathogen associated molecular patterns are released from bacteria, and viruses in the local areas of the brain and cause damage as well.
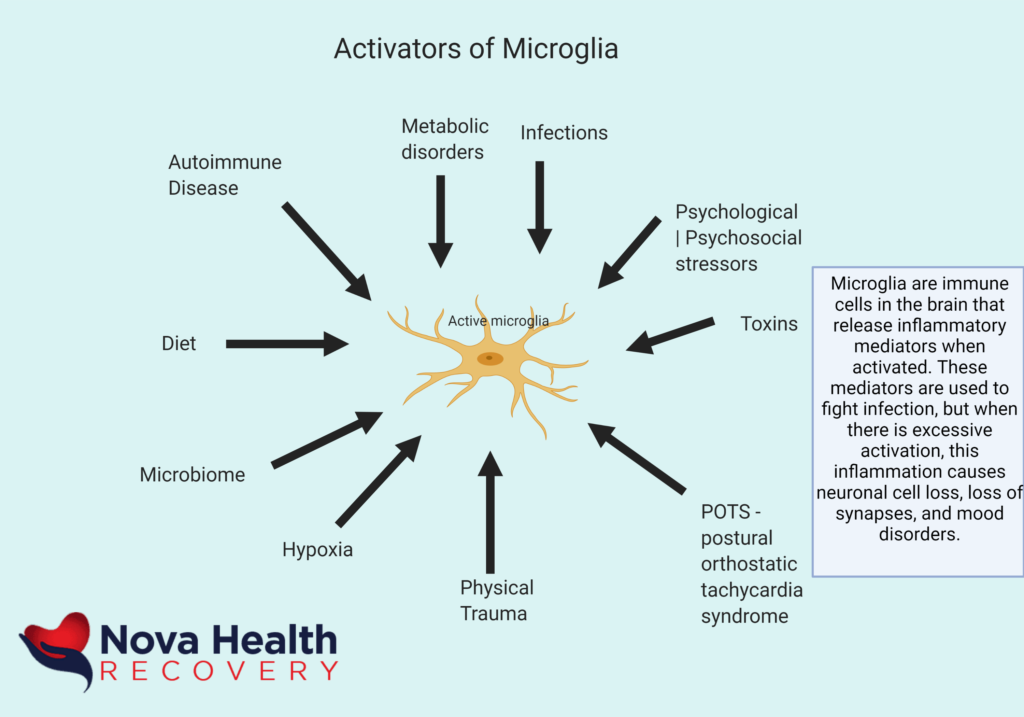
Damage to the neuron releases substances (DAMPS) that turn on microglia, which mediate inflammation. Microglia become activated (microgliosis) by:
- Increase in cell number
- Morphological Changes
- Phenotypic changes
- Protein Expression
- Release of immunoregulatory substances
The microglia monitor the environment (M1 state) in general and look for DAMPS and PAMPS, which when sensed, cause microglia to change their phenotype and become activated to spew out inflammatory particles.
POTS can be a result of Ehlers-Danlos Syndrome with hypermobility and autonomic instability that causes low blood pressure on standing, which decreases blood flow to the brain resulting in hypoxia, neuroinflammation, and chronic pain.
Pain and depression are symptoms of neuroinflammation.
Celiac disease and Lupus can produce neuroinflammation. Medications such as opioids can increase inflammation in the brain, resulting in more pain over time potentially. Infections such as chronic strep (PANDAS), EBV (Epstein Bar Virus), CMV (Cytomegalovirus), and Lyme disease can also cause inflammation in the brain. Concussions also result in a chronic inflammation of the brain over time. Epigenetics such as stress, sleep, medications, physical traumas can turn on or off genes in our system and affect our resilience and neural inflammation. Toxins due to lead from paint and gas, as well as mercury from fish, as well as Glyphosate, an antibiotic used for insect control, results in upregulated inflammation in the brain as well. Roundup is not poisonous to humans, but only to plants, but it does kill off our microbiome in the gut. The bacteria in that location, when healthy, prevent translocation of toxins into our body. Gut bacteria may be, in part, responsible for pain perception and central sensitization.
Ongoing damage to the musculoskeletal system such as arthritis, and chronic muscle damage will cause a continuous increase in inflammation that translates to the brain. Sleep apnea, when untreated, causes low oxygen in the brain and causes neuroinflammation and depression.
Metabolic changes, such as diabetes, with insulin and glucose regulation problems results in inflammation and cognitive errors.
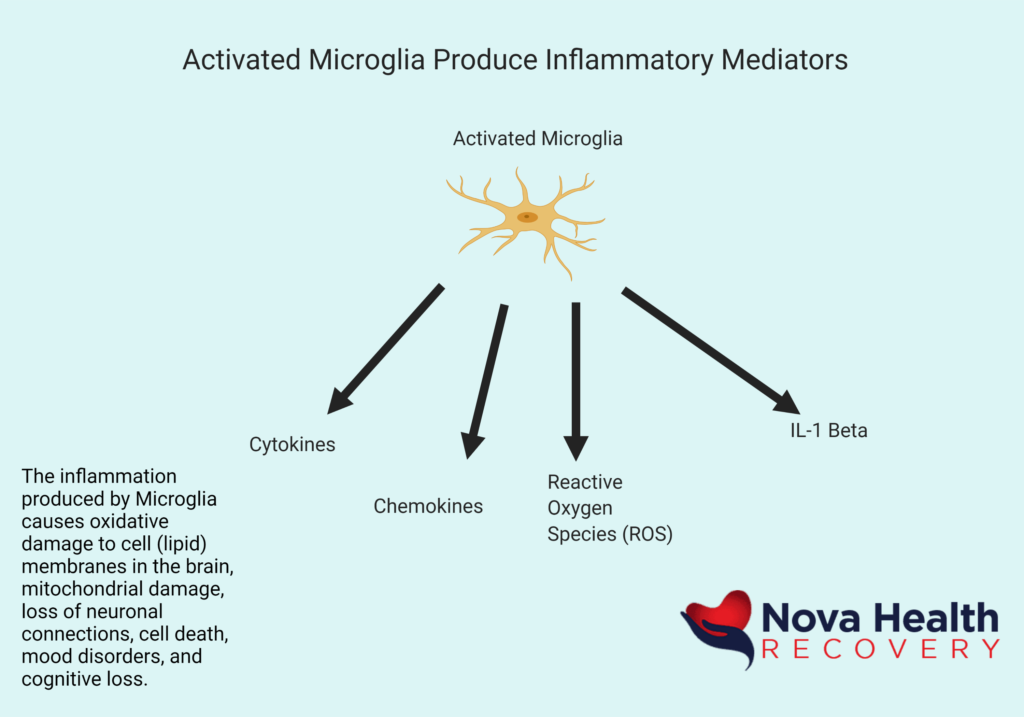
So, activation of microglia results in the production of neuroinflammatory mediators as below:
The symptoms associated with neuroinflammation and activated microglia with their products include:
- Anxiety
- Depression
- Fatigue
- Malaise
- Pain
- GI Dysfunction
- Fever
- POTS (postural orthostatic Tachycardia Syndrome)
- Sleep disturbances
- Endocrine disruption – cortisol and thyroid dysregulation
Chronic pain and depression are products of inflammation. Microglia become more inflammatory as we get older. More microglia are in an inflammatory phenotype as we age, they produce more pro-inflammatory cytokines (IL-6, TNF, IL-1), microglia produce fewer anti-inflammatory mediators (IL-10, BDNF, inhibitor of NF-kappa beta), and they have more of an exaggerated response to basic challenges. We see this in chronic pain, chronic fatigue, depression, neurodegeneration (Multiple sclerosis, Amyotrophic lateral sclerosis, Parkinson’s Disease), aging, and other conditions.
Chronic inflammation of the brain leads to these microglial changes and results in symptoms of cognitive loss and depression.
There is a strong correlation with brain aging, neurodegeneration, and redox imbalance along with low grade inflammation. Supplements can slow this process.
Neurodegeneration, which is found in depression and mood disorders, is characterized by chronic microglial overactivation and oxidative stress from mediators that they produce. It is the reactive oxidation species that damages other neurons and modulates microglial activity. The brain has low levels of antioxidants and is vulnerable to oxidative stress. We see a lot of oxidation in the brain with reactive oxidative species (ROS) and reactive Nitrogen Species (RNS) that originate from microglia and mitochondria in the brain. The RNS and ROS overwhelm antioxidants in the brain. This is overactivation of inflammation, production of oxidative species, and damage to cell membranes is the reason that replacement with antioxidants is so important.
Depression is progressive and neurodegenerative. We lose cognition and have worsened outcomes over time if depression is not treated rapidly and kept in remission. There can be increased inflammation, increased production of inflammatory mediators, increased quinolinic acid production, and neuronal damage when there is continued stress and lack of remission in depression and other mood disorders. Hence the need for rapid, aggressive therapies for depression and continued maintenance therapies.
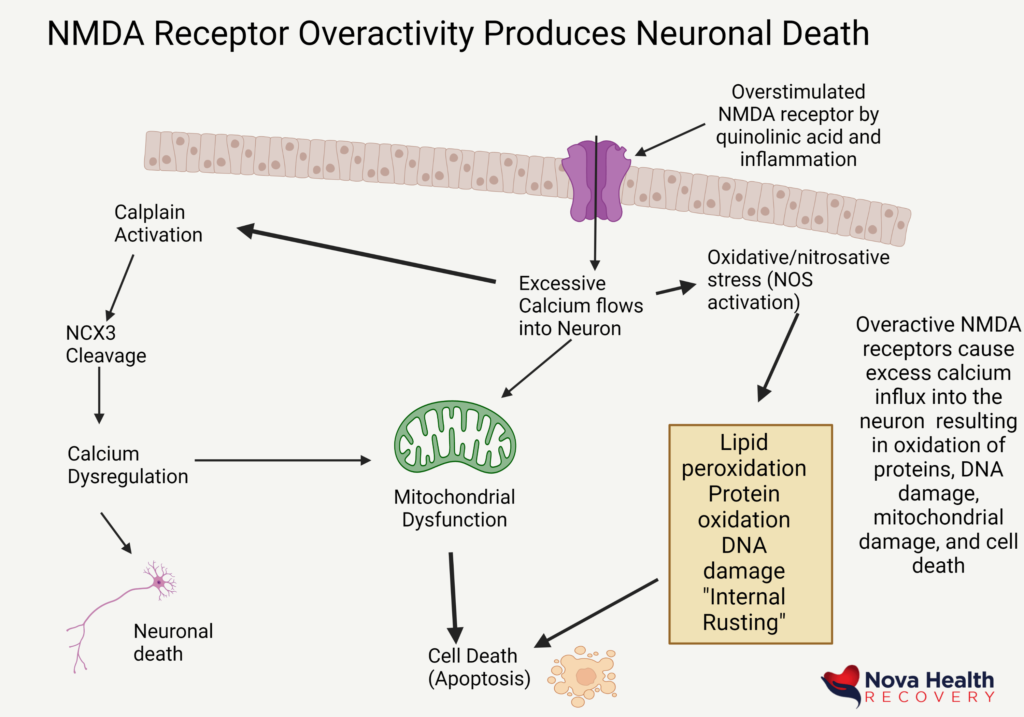
Microglial activation with increased inflammation in the brain leads to increased quinolinic acid production from tryptophan, an amino acid that is used to produce serotonin. Serotonin levels drop as a result. Increased quinolinic acid results in overactivity of the NMDA receptors in the brain which then causes neuronal cell hyperexcitability and death.
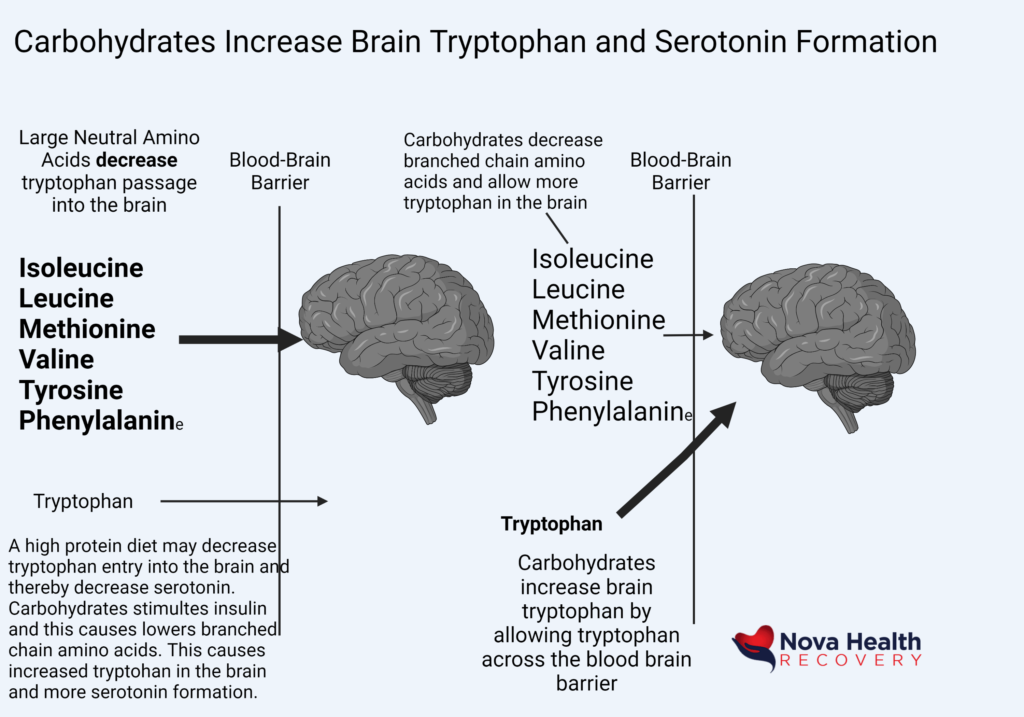
When we feel sad or depressed, carbohydrates are frequently indulged upon as they allow for insulin cycling and an increase of tryptophan flow into the brain. The tryptophan can then be used to produce serotonin – the molecule of happiness. The issue is that with increase inflammation, tryptophan may be converted to the brain-toxic quinolinic acid.
Excessive quinolinic acid and inflammation will over-activate the NMDA receptors , causing neuronal toxicity. NMDA receptors generally bind to glutamate, which is an important neurotransmitter of learning. This interaction must be brief in order for new synapses to form. When there is excess inflammation or quinolinic acid, excess glutamate becomes present and there is overstimulation of the NMDA receptors with hyperexcitability of neurons.
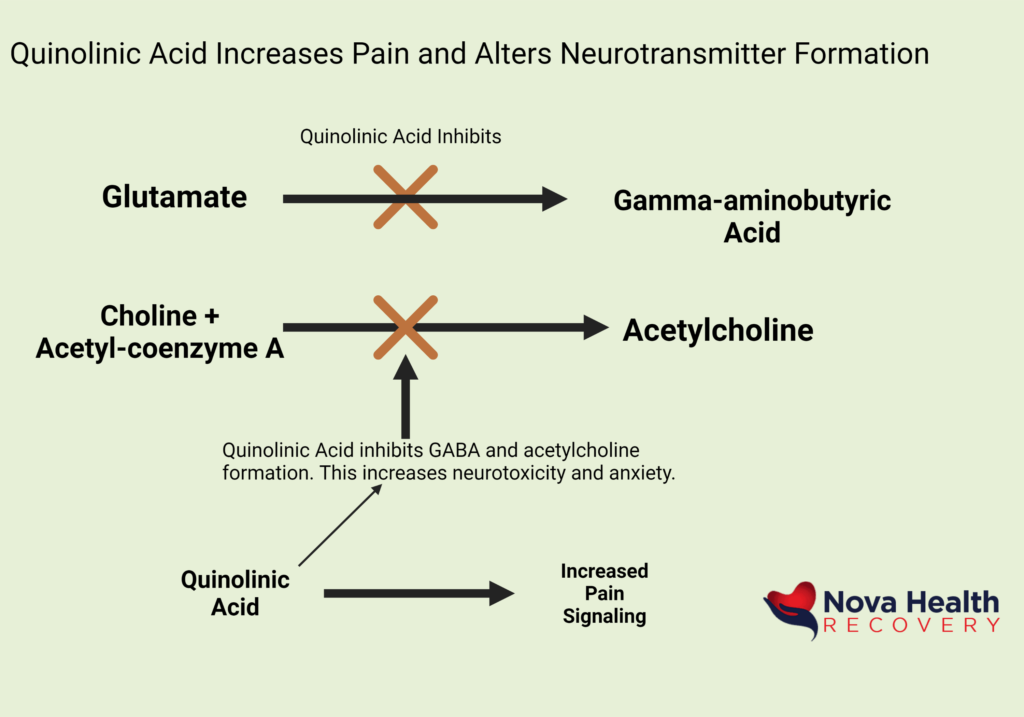
Excess quinolinic acid also prevents the production of GABA from Glutamate. GABA is a calming neurotransmitter that balances Glutamate. Also, quinolinic acid prevents acetylcholine formation, and also increases pain perception.
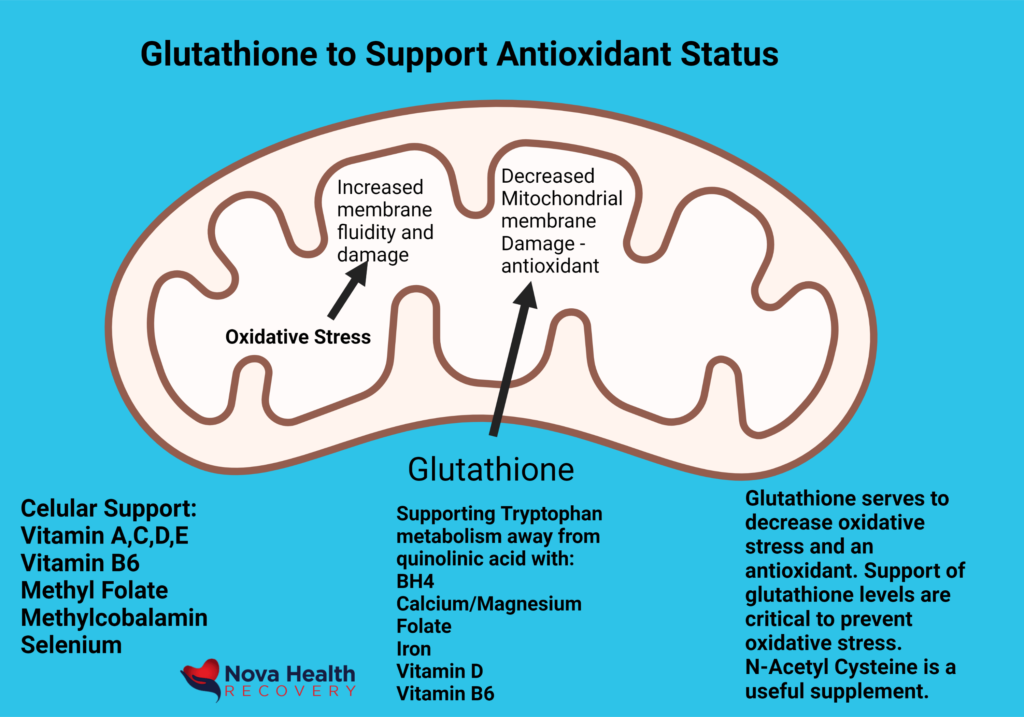
It is important to maintain the body’s antioxidant status when there is excess inflammation. Glutathione is the natural antioxidant molecule, and it runs low in times of oxidative stress. Excess oxidation damages cell membranes and mitochondrial function.